Pulseless Ventricular Tachycardia is a serious cardiac condition that requires immediate intervention and treatment. Along with medications, the pulseless V Tach treatment requires defibrillation. Originating in the ventricles, this condition is characterized by rapid heart rhythm. If not promptly treated, it can lead to something more serious, like a stroke or heart failure.
In the US, over 350,000 people die because of sudden cardiac arrests. The majority of deaths from SCA (Sudden Cardiac Arrests) are due to pulseless ventricular tachycardia. Therefore understanding how to identify and manage this condition is critical for healthcare professionals.
This blog will give you an in-depth understanding of the key aspects of pulseless ventricular tachycardia. You will get a comprehensive overview of the causes, symptoms and latest treatment protocols.
Master ACLS Now
Get ACLS certified with confidence
What is the pulseless ventricular tachycardia algorithm?
Pulseless Ventricular tachycardia is a complex cardiac arrhythmia that requires prompt medical intervention. The algorithm for pulseless VT allows streamlined intervention that is seamless and effective. These are the key steps in the pulseless ventricular tachycardia algorithm-
- Immediate Recognition and Activation of Emergency Response:
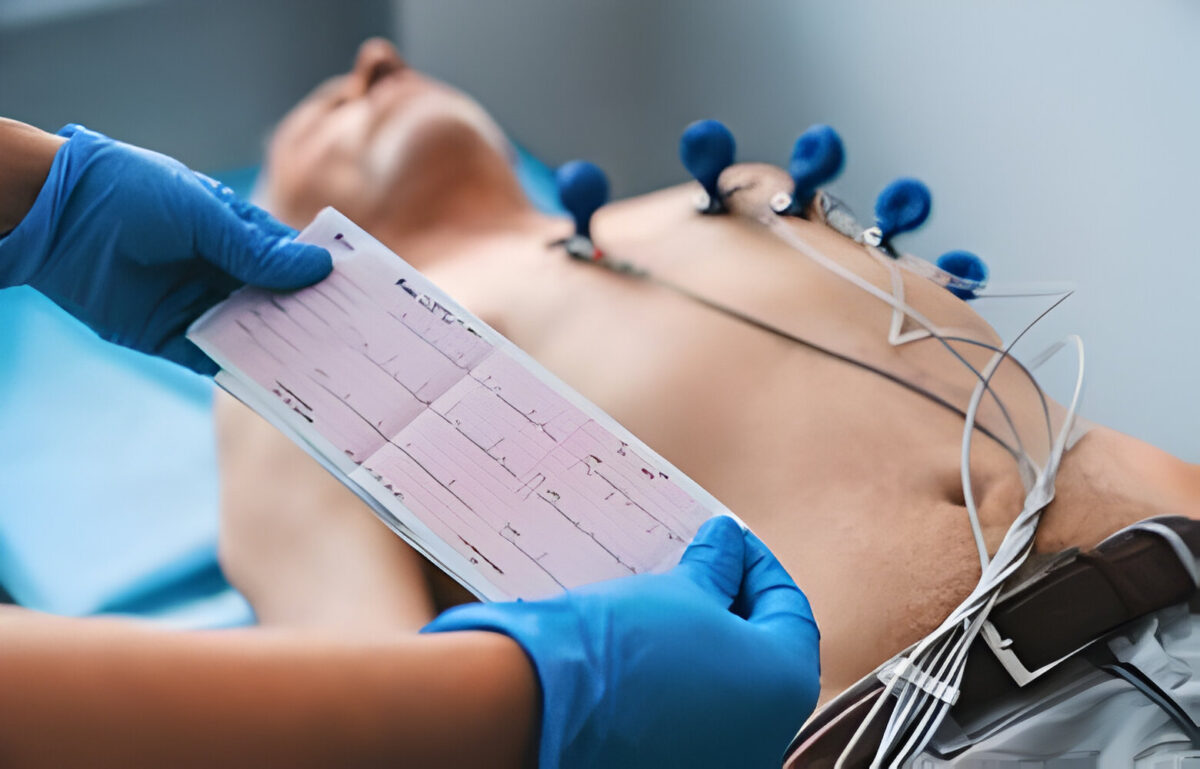
- Identify pulseless VT through ECG (rapid, regular wide-complex tachycardia).
- Check for pulse: If absent, confirm pulseless VT.
- Initiate Cardiopulmonary Resuscitation (CPR):
- Start high-quality CPR immediately.
- Ensure chest compressions are deep and at the correct rate (100-120 per minute).
- Defibrillation:
- Deliver a shock as soon as a defibrillator is available.
- Use the appropriate energy level for the defibrillator being used (e.g., 120-200J for biphasic, 360J for monophasic).
- Continue CPR:
- Resume CPR immediately after the shock.
- Continue for 2 minutes before rechecking rhythm and pulse.
- Medications:
- Administer epinephrine 1 mg IV/IO every 3-5 minutes during CPR.
- Consider administering amiodarone 300 mg IV/IO after the third shock, with a subsequent dose of 150 mg if VT persists.
- Advanced Airway and Ventilation:
- If trained and equipped, consider advanced airway management (endotracheal intubation or supraglottic airway).
- Ensure proper ventilation with a bag-mask device or advanced airway.
- Reassess and Continue Cycles:
- Reassess rhythm and pulse every 2 minutes.
- Continue cycles of CPR and defibrillation as indicated.
- Post-Resuscitation Care:
- Once return of spontaneous circulation (ROSC) is achieved, begin post-cardiac arrest care.
- Monitor and manage hemodynamic status, oxygenation, and ventilation.
- Consider targeted temperature management if indicated.
Read More: Confirming Placement Of Endotracheal Tube: Monitoring Techniques
Pulseless Ventricular Tachycardia: Signs to identify
In this condition, the heart’s ventricles beat rapidly but cannot produce an effective pulse. This leads to a lack of blood flow to the vital organs. It is important to identify the signs quickly, to provide the patients with best treatment. Here are the primary and most common symptoms of pulseless ventricular tachycardia-
- Loss of Consciousness:
- The patient may suddenly collapse or become unresponsive.
- Absence of Pulse:
- No detectable pulse despite rapid heart activity on the ECG.
- No Breathing or Abnormal Breathing:
- The patient may not be breathing or exhibit gasping (agonal respirations).
- Cardiac Arrest Symptoms:
- Cyanosis (bluish discoloration of the skin, especially the lips and fingertips).
- Unresponsive to verbal or physical stimuli.
- Electrocardiogram (ECG) Findings:
- Rapid heart rate typically over 100 beats per minute.
- Wide QRS complexes, often greater than 120 milliseconds.
- Monomorphic or polymorphic VT patterns.
- Absence of Normal Heart Sounds:
- Lack of normal heart sounds when auscultating the chest.
Read More: A guide to understanding ECG artifacts
Treatment and Management of Pulseless Ventricular Tachycardia
To restore effective heart rhythm and circulation, it is important to manage and treat pulseless vtach at the earliest. Healthcare providers need to abide by the established protocols to maximize chances of patient survival. These are steps to treat and manage Pulseless VT-
- Confirm pulseless VT through rapid assessment and ECG.
- Activate emergency medical services (EMS) immediately.
- Begin high-quality CPR. Ensure compressions are performed at 100-120 beats per minute and at least 2 inches deep.
- Deliver an immediate shock using a defibrillator.
- Use biphasic (120-200J) or monophasic (360J) settings as appropriate.
- Perform CPR for 2 minutes before checking the rhythm again.
- ‘Administer the medications (as per algorithm)
- Perform advanced airway management (Refer to the algorithm)
- Re-evaluate the patient’s rhythm and deliver shocks (as per requirement)
- Begin comprehensive post cardiac arrest
For a detailed insight into the steps of treatment, refer to the ACLS Algorithm for pulseless ventricular tachycardia.
Conclusion
The pulseless V Tach treatment demands rapid recognition and immediate intervention. By understanding the signs and symptoms, healthcare providers can effectively manage this life threatening condition. The chances of patient survival can be greatly enhanced by following the steps of pulseless ventricular tachycardia algorithm. Moreover, it is equally important to address the reversible causes and provide post-resuscitation care for long term recovery. Ultimately with the help of ongoing knowledge and practice, medical professionals can efficiently save lives and enhance patient outcomes.