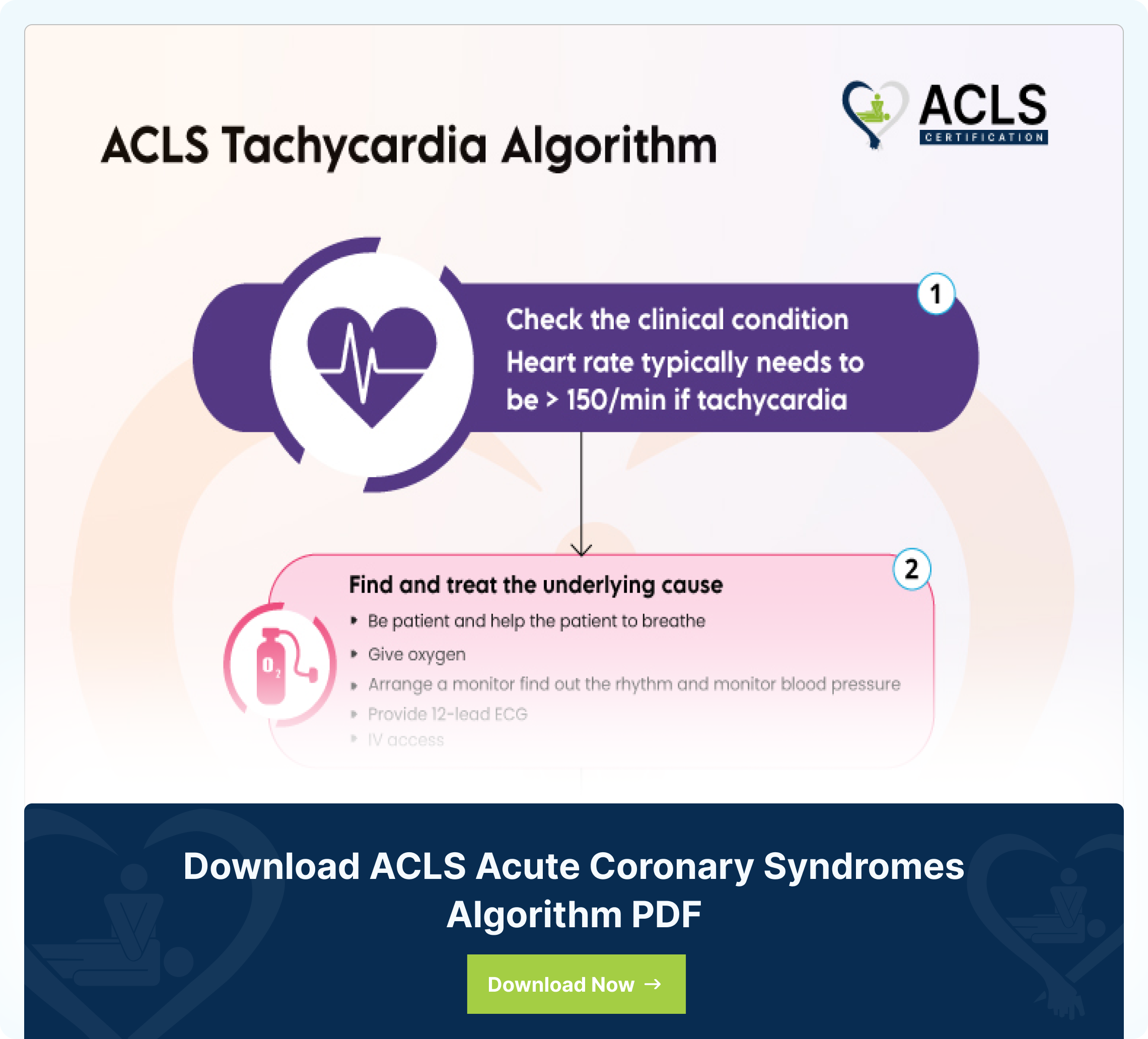
The ACLS (Advanced Cardiovascular Life Support) Tachycardia Algorithm is a structured set of protocols that helps the provider manage tachycardia patients. It helps manage an abnormally rapid heart rate in adults above the rate of 150 beats per minute. The algorithm offers a systematic way of grading and handling tachyarrhythmia to ensure proper and timely interventions are taken. The goal of all therapies is to improve and better patient outcomes. The algorithm is a successive set of steps that healthcare practitioners take when an adult patient presents with stable and unstable tachycardia. These processes involve adequate perfusion, initiating immediate synchronized cardioversion as well as administering antiarrhythmic drugs. Following these steps allows timely intervention and improves the survival rate of patients.
Step by step analysis of flowchart
- Assess Appropriateness for Clinical Condition:
-
- Determine the heart rate. Typically, tachyarrhythmia is greater than 150 beats per minute.
- If yes, proceed to the next step.
- Find and Treat the Underlying Cause:
- Identify and address the potential causes of tachycardia.
- Maintain an open airway and assist the patient to breathe, if necessary.
- Administer oxygen if the patient is hypoxemic.
- Cardiac Monitoring and Initial Assessments:
- Use a cardiac monitor to identify the rhythm and monitor blood pressure and oxygen saturation.
- Conduct a 12-lead ECG, if available.
- Establish intravenous (IV) access for potential interventions.
- Evaluate for Persistent Tachyarrhythmia Complications:
- Determine if the persistent tachyarrhythmia is causing complications such as hypotension, altered mental status, shock signs, ischemic chest discomfort, or heart failure.
- If yes for complications secondary to persistent tachyarrhythmia:
- If yes, consider synchronized cardioversion. Each device will have a recommended energy level to deliver the first shock. Please see the manufacturer manual.
- Consider sedation during the procedure.
- If the rhythm is regular and narrow, consider adenosine. First dose of adenosine is 6 mg IV push (rapidly). Always follow with an NS flush immediately after. The second dose of adenosine is 12 mg IV push. Always assess patients to determine if a second dose is necessary.
- If QRS is wide, consider interventions such as antiarrhythmic infusions.
- If regular and monomorphic, consider adenosine.
- If refractory, consider addressing the underlying cause, increasing energy levels during cardioversion, adding antiarrhythmic drugs, and consulting experts.
- Wide QRS > 0.12 seconds:
If yes, consider interventions for wide QRS complexes.- Consider adenosine only if the rhythm is regular.
- If refractory, consider addressing the underlying cause, increasing energy levels during cardioversion, adding anti-arrhythmic drugs, and consulting experts.
- Antiarrhythmic infusions for wide QRS tachycardia (stable) include:
- Procainamide IV (20-50 mg/min). Max dose is 17 mg/kg administered. Discontinue infusion if the patient becomes hypotensive, arrhythmia is resolved or subdued or the QRS increases by more than 50%. Maintain infusion with dose 1-4 mg/min.
- Amiodarone IV: 1st dose 150 mg over 10 minutes. Repeat if needed. Maintain infusion with 1 mg/min for the first 6 hours.
- Sotalol IV: 100mg or 1.5 mg/kg over 5 minutes
- If no, consider vagal maneuvers (if the rhythm is regular), adenosine, β-blocker, or calcium channel blocker, and consult medical experts.
- If refractory, then assess the underlying cause, increase the energy level, add anti-arrhythmic drugs, and consult medical experts.
Highlights of the ACLS tachycardia algorithm
- Early Recognition and Intervention:
Healthcare providers must identify signs of tachycardia and initiate the ACLS tachycardia algorithm while activating the emergency response system as necessary.
- Assessment and Basic Life Support:
This involves a rigorous evaluation of the patient’s stability, followed by appropriate interventions for regular narrow or wide-complex tachycardia. Basic life support interventions are provided based on the requirements, such as vagal maneuvers, adenosine administration, and the use of some anti-arrhythmic drugs.
- Advanced Cardiovascular Life Support (ACLS):
If patients are not stable, provide immediate synchronized cardioversion, anti-arrhythmic drugs, sedation, and seek expert consultation. Always make sure to have all the necessary equipment at bedside before initiating synchronized cardioversion.
- Identifying and treating reversible causes:
Recognizing and addressing reversible causes are crucial. It helps manage and improve all contributory factors, such as hypoxia, electrolyte imbalances, and drug toxicity.
- Post-Tachycardia Care:
Tachycardia care is administered initially before interventional stabilization and becomes post-tachycardia treatment after successful intervention and stabilization. This process involves constant monitoring, identifying the underlying causes, and finding best practices in patient outcomes.
- Recovery Measures:
Hospitals may incorporate interventions such as placing a patient in a recovery position. This method helps the airways stay closed and prevents inhalation in the unconscious but breathing patient.
- Refractory:
Refractory refers to a situation where a medical condition, such as tachycardia, does not respond to initial interventions or treatments. When tachycardia is considered refractory, it means that the initial treatments have not restored a normal heart rhythm. In such cases, aggressive interventions are required to manage the condition effectively.
- Wide QRS:
Wide QRS complex refers to a QRS interval that is greater than, or equal to, 12 seconds. You can measure the QRS complex on an electrocardiogram (ECG, also known as, EKG).
- Synchronized cardioversions:
Synchronized cardioversion is a medical procedure that helps restore a normal heart rhythm in individuals experiencing abnormal heart rhythms, especially tachycardias. The procedure delivers a carefully timed electrical shock to the heart while allowing the heart’s natural pacemaker to establish a more normal heartbeat.
Want to keep the highlights handy? Download the ACLS Tachycardia Algorithm now.
Download ACLS Tachycardia Algorithm PDF
Sources
- Advanced Cardiovascular Life Support Algorithms. Retrieved from https://www.ahajournals.org/doi/10.1161/circ.102.suppl_1.I-136
- Proper post-resuscitation care (PRC) has been shown to reduce mortality and morbidity. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4237286/#bib1
- Successful termination of the tachycardia by vagal maneuvers suggests AVNRT or CMT by an accessory pathway, whereas syncope suggests rapid SVT, atrial fibrillation with conduction over an accessory pathway, or concomitant structural cardiac abnormalities. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884443/
- Synchronized cardioversion is a procedure similar to electrical defibrillation in that a transthoracic electrical current is applied to the anterior chest to terminate a life-threatening or unstable tachycardia arrhythmia. https://www.ncbi.nlm.nih.gov/books/NBK482173/
- The most frequent reversible causes of CA with PEA as initial rhythm are commonly referred to by the mnemonic “4 Hs and 4Ts”: hypoxia, hypovolemia, hypo/hyperkalemia, hypo/hyperthermia, ca https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9485947/#B3
- A 2015 ILCOR Consensus on Science on this topic concluded that first aid providers should position unresponsive persons who are breathing adequately into a recovery position. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9065878/
- https://www.uptodate.com/contents/advanced-cardiac-life-support-acls-in-adults
- A normal QRS should be less than 0.12 seconds (120 milliseconds), therefore a wide QRS will be greater than or equal to 0.12 seconds. https://www.ncbi.nlm.nih.gov/books/NBK559054/#:~:text=A%20normal%20QRS%20should%20be,or%20equal%20to%200.12%20seconds
- https://pubmed.ncbi.nlm.nih.gov/29489237/#:~:text=Synchronized%20cardioversion%20is%20a%20procedure,threatening%20or%20unstable%20tachycardic%20arrhythmia
All ACLS Algorithms
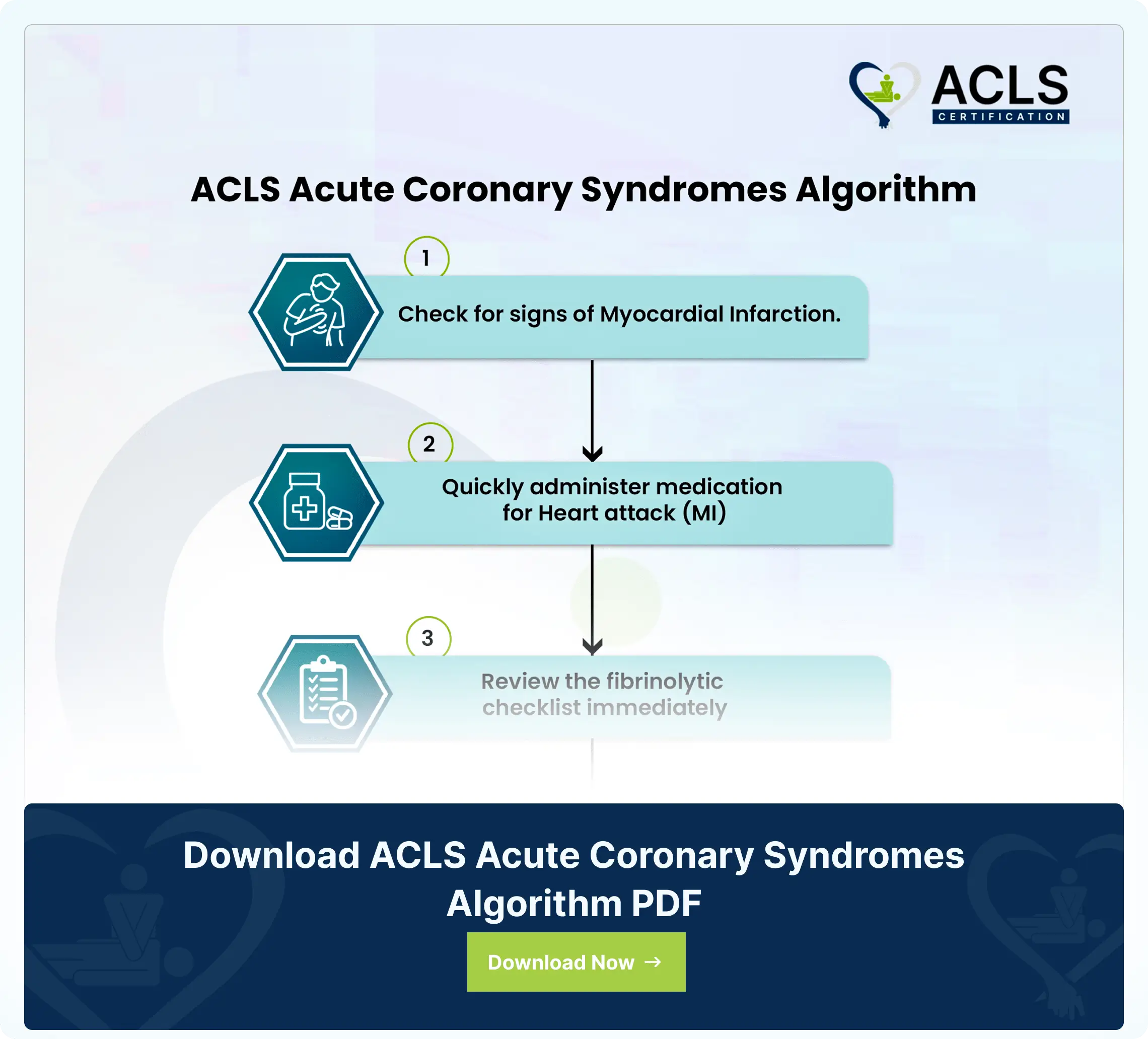
ACLS Acute Coronary Syndromes Algorithm
The ACLS Acute Coronary Syndromes Algorithm guides healthcare providers in the assessment, diagnosis, and treatment of patients with suspected or confirmed acute coronary syndromes
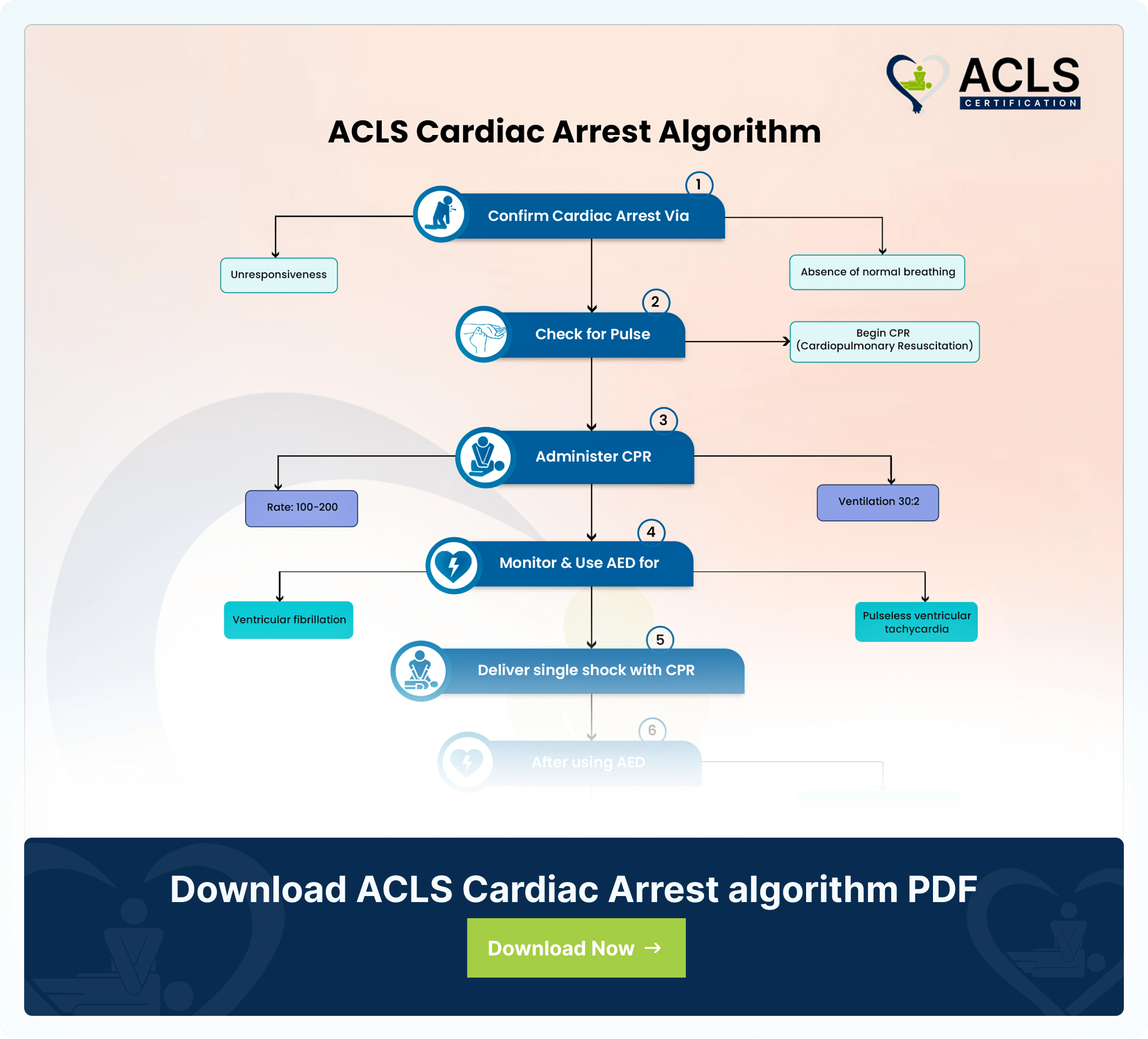
ACLS Cardiac Arrest Algorithm
The ACLS Cardiac Arrest Algorithm emphasizes CPR, defibrillation, drug therapy, and post-resuscitation care. It also highlights the importance of teamwork in optimizing outcomes during cardiac emergencies
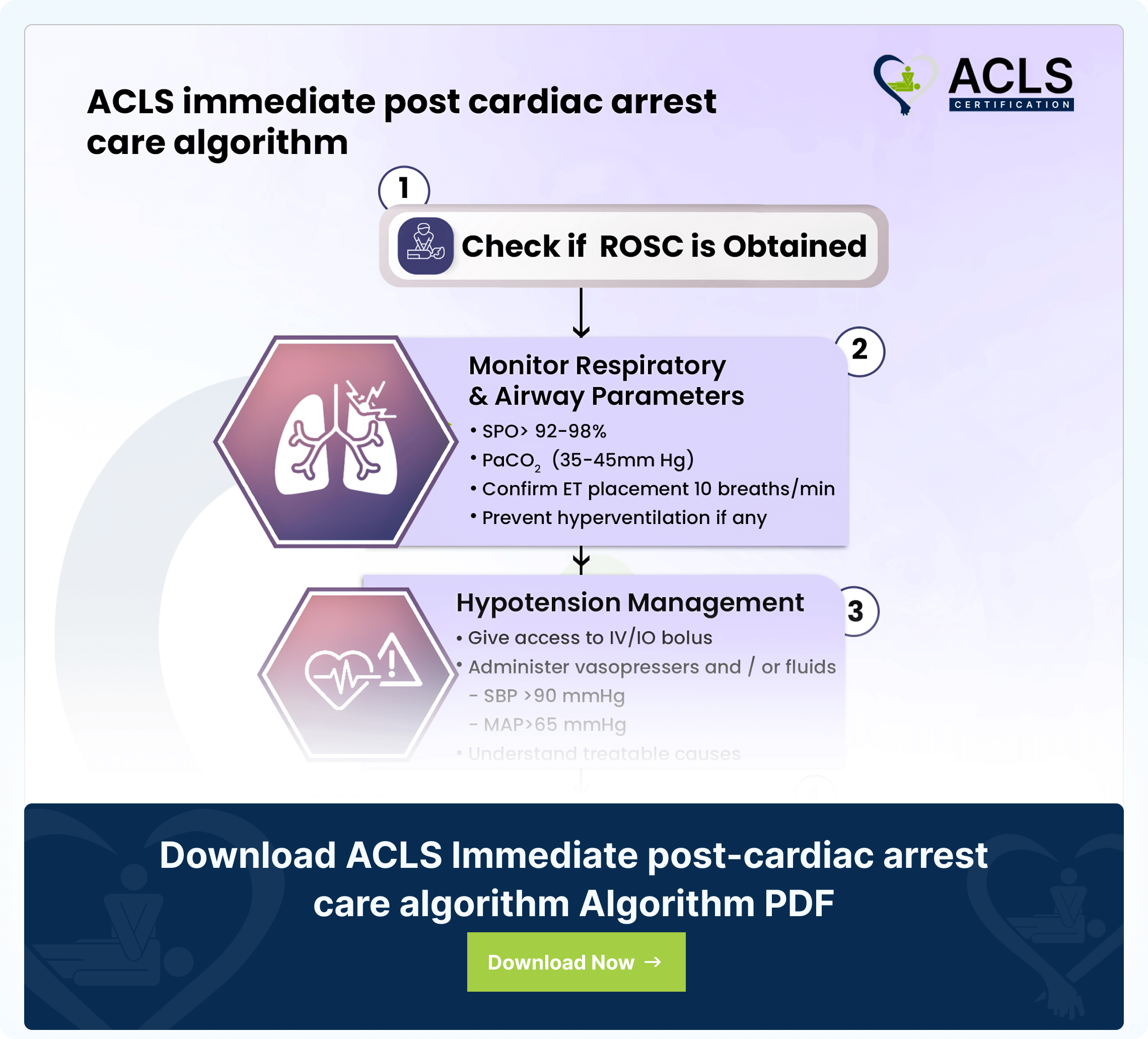
ACLS Immediate post-cardiac arrest care algorithm
The ACLS immediate post-cardiac arrest care algorithm guides critical interventions for patients post-resuscitation