Embarking on the journey of fibrinolytic therapy involves not just medical expertise but a strategic approach to ensure optimal patient outcomes. Did you know that every year, approximately 795,000 people in the United States suffer from a stroke? This could benefit from fibrinolytic therapy. It is crucial to have a comprehensive checklist that makes all the difference. Explore the key components of fibrinolytic checklist for more effective and timely stroke treatments:
Master ACLS Now
Get ACLS certified with confidence
Who may need prehospital fibrinolysis?
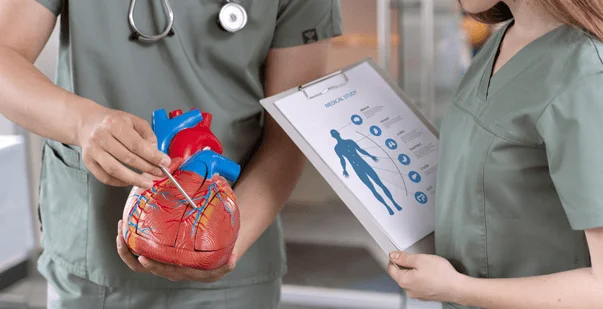
Prehospital fibrinolysis is a medical intervention for individuals experiencing acute myocardial infarction (AMI). Patients residing in remote or underserved areas require it. This helps in initiating the breakdown of blood clots, causing a heart attack, before the patient reaches a medical facility. This helps restore blood flow and reduces potential cardiac damage. Being highly crucial for emergency medical services (EMS) personnel, this carefully assesses the eligibility of patients based on specific criteria and ensures appropriate administration of prehospital fibrinolysis.
Read More: Stroke Management: ACLS Certification Guide
When should you not administer a fibrinolytic agent?
There are specific situations where the use of fibrinolysis may pose risks and potential harm to the patient. These fibrinolytic therapy contraindications are paramount for healthcare providers because they help them make informed decisions, ensuring patient safety. Here are situations when you must not administer fibrinolysis:
- Has a history of intracranial hemorrhage
- History of an ischemic stroke in the preceding three months
- Presence of a cerebral vascular malformation
- Symptoms or signs suggestive of aortic dissection
- Bleeding diathesis or active bleeding
- Facial trauma within the preceding three months
ACLS Fibrinolytic checklist
Systolic BP > 180 to 200 mm Hg or diastolic BP > 100 to 110 mm Hg
Right vs. left arm systolic BP difference > 15 mm Hg
History of structural nervous system disease
Stroke >3 hours or <3 months
Recent major trauma or surgery, including laser eye surgery
History of intracranial hemorrhage
Pregnant female
Serious systemic disease (e.g., advanced liver or kidney disease)
| Checklist | Yes | No |
| Heart rate>=100/min AND systolic BP<100mm Hg | Yes | No |
| Pulmonary edema (rales) | ||
| Signs of shock (cool, clammy) | ||
| Contraindications to fibrinolytic therapy | ||
| Required CPR |
If any of these items are checked yes, please consider transferring to the PPCI facility.
These absolute contraindications align with the 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction.
Contraindications and precautions of prehospital fibrinolysis
Introducing the considerations of contraindications and precautions is critical for ensuring the safe and effective administration of this intervention. While prehospital fibrinolysis can mitigate the impact of acute myocardial infarction (AMI), it is crucial to understand when to use it. Here are the precautionary measures for prehospital fibrinolysis:
Active Internal Bleeding: Fibrinolytic treatment is the dissolution of blood clots, which can worsen a present bleeding. Prehospital Fibrinolysis is contraindicated in the presence of active internal bleeding, like gastrointestinal bleeding, intracranial hemorrhage, or a recent major trauma. You need a careful assessment of the patient’s bleeding risk before considering the fibrinolytic agents.
Recent Major Surgery or Trauma: Inpatients who have recently undergone an operation or suffered from a significant trauma are more likely to have bleeding complications. Prehospital fibrinolysis is normally contraindicated in these cases because loss of control of bleeding will weigh more than the good of clot dissolution. A detailed analysis of the patient’s recent past medical history is important for the assessment of eligibility for fibrinolytic therapy.
Known Bleeding Disorders or History of Stroke: People with bleeding disorders, e.g., hemophilia, as well as those with cancer, cerebral infarction, or cerebral hemorrhage, can be at greater risk when treated with fibrinolytic agents. With this, the possibility of intensifying the bleeding issues makes prehospital administration of fibrinolysis not an option for these patients. Thoroughly assessing the patient’s medical history is key to the identification of contraindications and ensuring the safety of the intervention.
What are the timing and administration protocols?
An accurate time wall and strict adherence to the administration protocols are crucial in achieving the best outcomes of prehospital fibrinolysis. The time and administration processes have a precisely organized series of actions that ensure optimal effectiveness and patients’ safety. The process follows these below-mentioned key guidelines:
Recognition of Symptoms: Early detection of clinical symptoms pointing towards acute myocardial infarction (AMI) is a must. It is crucial to take action by providing emergency medical service (EMS) to assess and identify the patients eligible based on symptoms as well as the first ECG of the heart.
Contacting Medical Control: Once a suitable candidate is identified, paramedics must call medical control or the receiving hospital to verify his or her eligibility and obtain permission for the fibrinolysis. The last step is to have an online consultation with a health professional to receive instructions on administration.
Preparation of Fibrinolytic Agent: After obtaining approval, the fibrinolytic agent is now processed following recommended guidelines. This involves determining the right dose considering the patient’s weight and the drug being instantly available for administration as the patient arrives at the hospital.
Administration On-Site: The fibrinolytic therapy is administered on-site, usually through an IV setup. The procedure entails adhering strictly to the drug infusion rate recommendations and observing the patient for any adverse effects while the medication is being administered and after that.
Transport to the Hospital: After transferring the patient to the hospital with coronary angiography capabilities for further evaluation and possible additional interventions, the time of transport is critical. While you must ensure to avoid any delays and highlight (or stress) the significance of logistics and communication.
Ongoing Monitoring: It is crucial to continuously monitor the patient’s vital signs, ECG, and entire clinical condition during transportation and at the hospital. This is helpful in finding out any complications in time and, therefore, early intervention.
The timing and administration protocols highlight the importance of prehospital fibrinolysis and a closely coordinated team of healthcare professionals to ensure the best outcomes for patients with acute myocardial infarction.
Read More: ACLS Certification: What is it and who needs it?
Conclusion
The fibrinolytic checklist is a vital tool for healthcare providers, and by exploring patient eligibility criteria, administration protocols, and more, it underscores the significance of a strategic approach and ensures optimal outcomes. The comprehensive checklist enhances the efficiency and effectiveness of fibrinolytic interventions.