Atrial fibrillation poses a significant challenge and involves erratic atrial contractions that cause a big stir in the normal cardiac rhythm. Did you know that more than 33 million individuals suffer from arrhythmia, which has a widespread impact on cardiovascular health? Afib is more than an irregular heartbeat causing dizziness and palpitations. In this blog, learn the causes, symptoms, and treatment of ACLS atrial fibrillation.
Master ACLS Now
Get ACLS certified with confidence
What is atrial fibrillation?
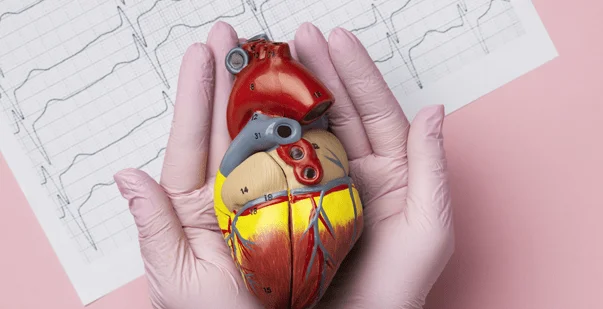
Atrial fibrillation (AF) is an abnormal cardiac rhythm that results from the erratic firing of multiple cells in the upper chambers of the heart and causes the atria to shake disorderly and without the desired smooth pumping activity. Atrial fibrillation (AF) is the most common sustained form of cardiac arrhythmias on a clinical level, and this condition is associated with a high risk of thromboembolism, strokes, dementia, falls, and death.
Read More: ACLS Certification in Utah
What are the causes of atrial fibrillation?
The electric impulses that cause the heart muscle to pump start in the sinoatrial node, the portion of the heart that is responsible for starting the atrial pumping. This portion of the heart is located in the upper right chamber of the heart, called the right atrium. The atrioventricular node sends a signal to both the right atrium, which are referred to as the atria, and the left atrium.
The signal makes these chambers contract, and then, in sequence, the ventricles, the bottom chambers, will contract. This is the process through which the upper chambers of the heart suck in blood, which in turn pumps them to the ventricles of its lower chamber. The impulse is then relayed along the heart to the ventricles, which send them the contraction signal.
In atrial fibrillation, cardiac conduction is dysfunctional due to aberrant electrical signals coming out of the atria, which hamper the normal heart rhythm. These signals or triggers, which the brain usually sends to the upper chambers to pump blood regularly and synchronously, are disrupted, so the lower chamber works extra hard to compensate.
When the muscle tone of the heart or its electrical activity is damaged, the normally regular heart pumping operation will be chaotic and fail quickly. This damage is most typically linked with other diseases, such as high blood pressure and heart disease.
Read More: Acls promo code
Changes in heart tissue
As the heart ages or heart disease occurs, secondary infections and genetic factors can affect the heart tissue and make local cells contract, resulting in an abnormal rhythm. You can alter heart tissues in several ways, affecting the ability of your heart to contract, like fibrosis, inflammation, stretching, thinning, or swelling of the heart walls.
Changes to the heart’s electrical signaling
Individuals with atrial fibrillation experience a very fast and erratic heartbeat, which signals an immediate attack. On the other hand, electrical signals from this irregular rhythm may as well make the heart beat slower or faster while under excessive strain. In certain circumstances, electrical signals may validate an untoward round, instructing the heart to beat all the time. This may eventually result in the formation of the irregular, rapid heart rate that results in atrial fibrillation. This condition is a major cause of stroke, heart failure, and other life-threatening events.
Read More: What Are the Psychological Aspects of Patient Care in ACLS?
What are the symptoms?
The symptoms of ACLS AFIB are the following:
Chest discomfort
Respiratory distress
Light-headedness and loss of consciousness
Hypotension
Pulmonary edema
As a result, it is crucial to track the symptoms and treat the concern accordingly.
What is ACLS treatment for AFIB?
A synchronized electrical shock method follows, which is called direct cardioversion. While attempting to submit a shock, there is a high chance that the SA node will re-engage and the individual will resume a normal heartbeat rhythm. You can administer anesthesia to reduce the painful nature of the operation for outpatients.
Start anticoagulation for patients with AF containing a new onset lasting for more than 48 hours prior to any electrical cardioversion. This is to avoid clots within the atria. From there, they may potentially lodge in any other part of the body, such as in the coronary arteries, which may lead to a heart attack or stroke, or in the lungs with a pulmonary embolism. On other occasions, the reactions following cardioversion can be transitory, or ablation might be an alternative.
The instruments used for the performance of ablation are similar to the ones used in the catheterized cardiac environment. At the end of the stage, a catheter has access to the femoral artery. Then the catheter is carefully navigated into the right part of the heart.
To try and displace those cells with odd impulses, the cardiologist uses the angiography in the atrium of the heart. The catheter heats, burns, or destroys them. With such cells no longer interrupting the SAN, the patient frequently changes to a more regular rhythm. Ablation has a much higher probability of being successful than cardioversion.
Read More: ACLS certification: What is it, and who needs it?
Conclusion
ACLS atrial fibrillation is a common cardiac arrhythmia that affects the majority of individuals worldwide. It is crucial to be vigilant about the symptoms and perform timely interventions. ACLS is crucial in ensuring a proficient response to restoring cardiac rhythm and improving patient outcomes.