Table Of Content(s)
- Introduction
- Anatomy of the Patient’s Airway
- Common Airway Obstructions
- Basic Airway Maneuvers
- Airway Adjuncts
- Bag-Valve-Mask (BVM) Ventilation: A Crucial Lifesaving Tool
- Final Thoughts
Airway management adults is an essential skill in healthcare, often acting as the foundation of emergency medical treatment. It covers many methods and procedures to guarantee a patient’s airway remains open and functioning. From simple movements to more complex operations, airway management is crucial in situations ranging from regular treatments to life-threatening emergencies.
The difference between life and death may be found in the capacity to evaluate and control compromised airways rapidly. Mastery of these abilities is not just a need but also a duty that will significantly affect patient outcomes as medical professionals. Explore with us the complex field of airway management, where every breath matters and lifesaving strategies wait for your learning.
Master ACLS Now
Get ACLS certified with confidence
Anatomy of the Patient’s Airway
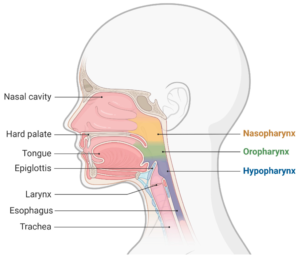
The human airway has two sections: the upper airway includes the nose, mouth, pharynx, and larynx, and the lower airway includes the trachea and bronchi. Each component is important for lung protection and breathing.
The nose moistens, heats, and filters air. The mouth makes larger air volumes during exercise or tension possible. The pharynx links the nose and mouth to the larynx. It also helps one swallow. The larynx holds the voice cords and protects the lower airway. Rising to the lungs, the trachea—a tube-like structure—carries air. Branching out from the trachea, bronchi provides air to many lung regions.
Common Airway Obstructions
Obstructions of the airways may cause major risks and need quick detection and treatment. Recognizing the common causes of airway blockages is crucial for effective intervention. Here are the typical obstructions encountered in airway management for adults.
-
Foreign Objects
Inhaling or ingesting objects, especially in children, may obstruct the airways. Children’s narrower airways make them more likely to choke on toys or small items. Adults also experience this, usually with dental appliances or food particles.
-
Respiratory Conditions
Asthma and Chronic Obstructive Pulmonary Disease (COPD) are key causes of airway obstruction. Asthma causes coughing and wheezing by enlarging the airways and producing extra mucus. Often caused by chronic bronchitis or emphysema, COPD restricts airflow and results in shortness of breath and chest discomfort.
-
Sleep-Related Obstruction
Adults’ most frequent chronic upper airway condition is obstructive sleep apnea (OSA). It may substantially interfere with breathing patterns and sleep and originate from laryngeal problems.
-
Allergic Reactions
Severe allergies may rapidly block airways. Foods like peanuts or insect stings might set off swelling that blocks or narrows the airway. If not treated quickly, this response may be fatal.
Read More: How to master BVM Ventilation?
Basic Airway Maneuvers
Basic airway maneuvers are essential techniques for opening and maintaining a clear airway in unconscious or unresponsive patients. They are often the first steps in emergency airway management.
-
Head-Tilt Chin-Lift Maneuver
One of the pillars of airway opening techniques is the head-tilt chin-lift. With tongue and soft tissue manipulation, this move seeks to free the airway. Let’s look at the ways to do it:
- Place one hand on the patient’s forehead.
- Gently push to tilt the head back.
- Use your other hand’s fingers to lift the chin.
- This action pulls the tongue forward, away from the throat’s back.
- The airway opens as a result of this movement.
- For suspected neck injuries:
- Maintain a neutral spine position
- Focus on lifting the chin
- Keep the head aligned with the body
- Avoid tilting the head back
This technique is fundamental in BLS airway management. Additionally, it is the first step in addressing airway obstruction.
-
Jaw Thrust Maneuver
Another essential airway opening method is the jaw thrust maneuver, which is particularly helpful when a head-tilt chin-lift is not advised due to neck injury concerns.
- Start this move by kneeling at the top of the patient’s head.
- Put your hands on each side of their face, fingers behind the jaw’s angle.
- Lift the jaw softly forward and upward. This motion lifts the tongue away from the rear of the neck and forwards the jaw.
- If no neck injury is anticipated, the jaw push may be performed alone or with a small head tilt.
This approach is quite helpful in trauma scenarios where keeping spinal alignment is very important. Basic airway management depends critically on the jaw push, much as the head-tilt chin-lift.
-
Cervical Spine Immobilization
Management of patients with possible neck injuries depends critically on cervical spine (c-spine) immobilization. Some neck movement brought on by airway manipulations raises the risk of further damage. Stabilizing the c-spine safeguards the patient and reduces this danger.
- If feasible, use manual in-line stabilization with enough staff to keep the patient’s head and neck steady.
- Stay clear of mechanical limitations, as they could raise intracranial pressure and compromise airway management.
- If a cervical collar is present, the front portion may need to be removed or opened to control the airway.
- While simple airway techniques are carried out, manual stabilization should continue to guarantee the protection of the C-spine.
These basic airway management techniques form the foundation of emergency airway care. To stay competent, healthcare professionals should routinely do these maneuvers. Always be ready to escalate care if these basic maneuvers fail to meet the patient’s needs. These methods may greatly enhance patient outcomes with correct training and use in many emergencies.
Airway Adjuncts
Devices used to preserve or open the airway of a patient are called airway adjuncts. When simple movements are insufficient, they are truly vital instruments. The basic airway adjuncts and their correct use are:
-
Oropharyngeal Airways
A necessary basic airway adjunct is a curved plastic device called an oropharyngeal airway (OPA). These instruments prevent the tongue from obstructing the throat, therefore preserving an unobstructed airway in unconscious patients. Measuring from the mouth’s corner to the earlobe can help you first choose the appropriate size for an OPA.
After orienting the OPA 180 degrees as it passes the soft palate, insert it with the curvature toward the mouth. Ideally, the flange rests on the lips. Opas only fit very unconscious individuals as they may cause gagging in those with intact reflexes. Regular monitoring is important after placement to ensure the patient’s comfort and safety.
Additional Note:
Patients with an intact gag reflex should avoid OPAs, as they could induce laryngospasm or vomiting. They are most helpful in profoundly unconscious patients as part of airway obstruction management. After insertion, the patient should always be constantly monitored and ready to withdraw the OPA if the patient starts to gag or regain consciousness.
-
Nasopharyngeal Airways
Another type of airway adjunct utilized in basic airway adjuncts is nasopharyngeal airways (NPAs). These soft, tube-like devices pass via the nose into the pharynx. In semi-conscious individuals, NPAs are tolerated better than OPAs and may be utilized when mouth opening is limited.
Measure from the tip of the nose to the earlobe to size an NPA. Following the floor of the nasal cavity, lubricate the NPA, then gently enter it into the bigger nostril opening. The flared end should lay against the nostril aperture.
Patients suspected of skull base fractures should not use NPAs. Although usually safer than OPAs, sometimes they might induce nosebleeds. Maintaining airway patency in emergency treatment depends much on both OPAs and NPAs.
Read More: CPR VS BLS: What’s the difference?
Bag-Valve-Mask (BVM) Ventilation: A Lifesaving Tool
Three basic components make up the BVM: a one-way valve, a self-inflating bag, and a face mask. The bag draws in new air or oxygen as it recoils after every press. The valve prevents expelled air from finding re-entry into the bag. Different patients will fit the many sizes of the face mask.
-
Proper Technique
To properly operate a BVM, put yourself at the patient’s head. With your other fingers lifting the jaw in an “E,” hold the mask with your thumb and index finger, producing a “C” shape. For adults, squeeze the bag with your other hand, providing one breath every five to six seconds. Look for chest rise to guarantee appropriate breathing.
-
Common Issues and Troubleshooting
If you don’t see a chest rise, check for a mask seal, reposition the airway, or consider using an airway adjunct. Increased stomach inflation caused by too much breathing raises aspiration risk. If this happens, moderate your pace and cut volume.
-
Importance of Proper Seal and Rate
Successful ventilation depends on a good mask seal. Without it, the patient runs out of oxygen, and air escapes. Maintaining the proper breathing rate guarantees the best oxygenation and helps to avoid hyperventilation. Regular practice keeps one proficient in this essential ability.
-
Monitoring and Reassessment: Keeping a Watchful Eye
Continuous monitoring is key to effective airway management.
- Watch for chest rise and fall, listen for breath sounds, and feel for air movement.
- Use pulse oximetry to track oxygen levels and heart rate.
- Regular reassessment helps catch changes quickly.
- Look for signs of improvement, such as easier breathing, better color, and increased alertness.
These indicate that your interventions are working. On the flip side, watch for red flags. Increased breathing work, dropping oxygen levels, or worsening consciousness may signal deterioration.
Don’t rely solely on machines. Use your senses, too.
- Feel the patient’s skin for temperature and sweat.
- Listen for changes in breath sounds or new noises.
- Watch for the use of accessory muscles or changes in posture.
Stay vigilant and be ready to adjust your approach as needed. Quickly recognizing problems leads to faster, more effective interventions.
Final Thoughts
For those working in the medical field, mastering airway management adults is very important and may make all the difference in an emergency. This essential ability calls for knowledge, experience, and fast thinking. Understanding the anatomy, spotting any blockages, and using the right treatments can help you keep a patient’s airway open and guarantee adequate oxygenation.
Still, reading about airway management is just a starting point. To really shine, look for practical instruction and certification. Regular practice and continuous learning will help you maintain your abilities so they are fresh and ready for the most required use.