Table Of Content(S)
- What is tension pneumothorax?
- Elaborate on the Tension Pneumothorax Treatment
- Tension pneumothorax Signs & Symptoms
- Conclusion
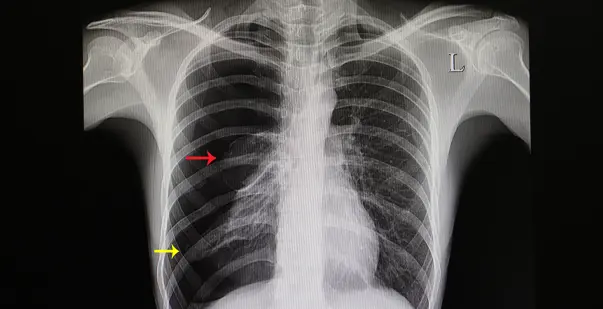
Tension Pneumothorax is a potentially life threatening condition that is marked by accumulated air in the pleural space. The pleural space is the area between the lungs and the chest wall. When air gets trapped here, it creates excessive pressure impairing normal respiratory and cardiovascular function. This being an emergency, needs immediate intervention, Without prompt treatment, the buildup of pressure severely affects the lungs, obstructing blood flow to the heart.
To recognize the early signs and symptoms, understanding tension pneumothorax is a must. Symptoms often include sharp chest pain, breathing difficulty, rapid heart rate and bluish-pale skin. In this blog, we will explore the causes and risk factors associated with tension pneumothorax. Read along to get valuable insights into the management of tension pneumothorax and its implications for patient care.
Master ACLS Now
Get ACLS certified with confidence
Tension Pneumothorax Signs & Symptoms
Recognizing the signs and symptoms of tension pneumothorax is critical. This aids in timely intervention and effective treatment. This condition can escalate rapidly and lead to severe respiratory and cardiovascular problems. Understanding the key indicators can help professionals and first responders identify and manage this medical emergency. Here are the primary signs and symptoms of tension pneumothorax:
Read More: Identifying and Treating Atrial Fibrillation (AFib or AF)
- Sudden Sharp Chest Pain: The most common symptom, often localized on the side of the affected lung, can be intense and may worsen with breathing or coughing.
- Severe Shortness of Breath: Rapid onset of difficulty breathing due to reduced lung capacity and impaired gas exchange. This symptom often escalates quickly.
- Rapid Heart Rate (Tachycardia): The heart rate increases as the body tries to compensate for decreased oxygen levels and reduced cardiac output.
- Hypotension (Low Blood Pressure): Due to decreased venous return to the heart, blood pressure can drop, leading to shock if untreated.
- Distended Neck Veins: Elevated pressure in the chest can cause the veins in the neck to become visibly swollen and distended.
- Tracheal Deviation: The trachea may shift away from the affected side due to pressure buildup, a late and serious sign indicating significant displacement of thoracic structures.
- Cyanosis: A bluish tint to the skin, lips, or fingernails indicates severe oxygen deprivation and requires immediate action.
- Decreased or Absent Breath Sounds on the Affected Side: During physical examination, reduced or absent breath sounds over the affected lung can be detected with a stethoscope.
- Hyperresonance to Percussion: The affected side of the chest may produce a hollow, drum-like sound when tapped, indicating the presence of trapped air.
- Anxiety and Restlessness: Patients may appear extremely anxious, restless, or agitated due to difficulty breathing and lack of oxygen.
- Sweating (Diaphoresis): Excessive sweating can occur as the body reacts to the stress of decreased oxygen levels and increasing discomfort.
What is Tension Pneumothorax Treatment?
Immediate treatment following the diagnosis of tension pneumothorax is a must. The primary goal of the treatment is to decompress the pleural space. This is followed by addressing additional and underlying issues. Here’s an overview of the standard approaches used to manage tension pneumothorax:
Immediate Needle Decompression: This is the first and most urgent step in treating tension pneumothorax. A needle is inserted into the pleural space, usually at the second intercostal space in the midclavicular line, to allow trapped air to escape. This procedure rapidly relieves the pressure and can provide immediate symptom relief.
Chest Tube Insertion: After initial needle decompression, a chest tube is typically inserted to continuously drain air or fluid from the pleural space. The chest tube is placed between the ribs into the pleural cavity and connected to a drainage system. This allows for ongoing decompression and helps prevent the recurrence of pneumothorax.
Read More: Synchronized Cardioversion ACLS Cheat Sheet
Supplemental Oxygen: Providing supplemental oxygen helps to increase oxygenation and support respiratory function. This is particularly important if the pneumothorax has led to significant respiratory distress or hypoxemia.
Mechanical Ventilation: In severe cases where the patient’s respiratory function is critically compromised, mechanical ventilation may be required. This involves the use of a ventilator to assist with breathing and ensure adequate oxygen delivery to the body.
Surgical Intervention: In some instances, especially if the pneumothorax is recurrent or associated with underlying lung pathology, surgical intervention may be necessary. Procedures such as video-assisted thoracoscopic surgery (VATS) or thoracotomy can be performed to repair lung injuries or remove persistent air leaks.
Treating Underlying Causes: Identifying and addressing the underlying cause of the tension pneumothorax is essential for preventing recurrence. This may involve treating conditions such as lung infections, trauma, or underlying lung diseases that contributed to the development of the pneumothorax.
Monitoring and Follow-Up Care: After initial treatment, close monitoring of the patient’s respiratory and cardiovascular status is critical. Follow-up care may include repeat imaging studies to ensure the pneumothorax is resolving and to monitor for any complications.
Pain Management: Effective pain control is important for patient comfort and to facilitate breathing. Analgesics or regional anesthesia may be administered to manage pain associated with the pneumothorax and its treatment.
Conclusion
Being a potentially fatal medical condition, prompt intervention is critical for someone diagnosed with Tension Pneumothorax. The ability to identify the signs exhibited by this condition ultimately saves lives and improves outcomes for those affected. A proper understanding of the condition’s mechanisms, manifestations, and treatment protocols, can help deliver the best care to someone experiencing this acute health threat. During such critical medical challenges, only continued education can truly and significantly make a difference.