Table Of Content(s)
- Introduction
- What are the different types of POTS (Postural Orthostatic Tachycardia Syndrome)?
- What are the steps to treat and manage POTS?
- What is the link between POTS and other underlying health conditions?
- Conclusion
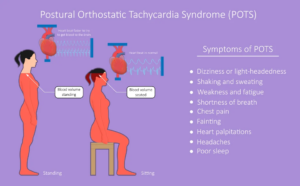
Imagine this, you stood up, you are feeling lightheaded and then you faint. For people with Postural Orthostatic Tachycardia Syndrome (POTS), the situation is almost similar. For most of them, this is an everyday reality.
But what exactly is POTS?
POTS or Postural Orthostatic Tachycardia is a form of dysautonomia that affects blood flow. This makes the heart beat fast when standing. But what many don’t know is that POTS has different types, each with its own set of challenges.
Over 1 to 3 million people in the US suffer from POTS. Without the understanding of the types of POTS, it is impossible to diagnose the condition and treat it. Explore the variants on Postural Orthostatic Tachycardia Syndrome and what makes each one unique.
Master ACLS Now
Get ACLS certified with confidence
What are the different types of POTS (Postural Orthostatic Tachycardia Syndrome)?
There are several different types of Postural Orthostatic Tachycardia Syndrome (POTS). They have their distinct characteristics and causes. The most common types include:
1. Neuropathic POTS
- Cause: Damage or dysfunction in the small nerve fibers that control blood flow and vessel constriction in the legs.
- Symptoms: Blood pools in the lower extremities. This leads to lightheadedness, dizziness, and a rapid heart rate when standing.
2. Hyperadrenergic POTS
- Cause: Overactivity of the sympathetic nervous system results in excess norepinephrine (adrenaline) in the blood.
- Symptoms: Palpitations, anxiety, high blood pressure, and tremors are common. This type is also linked with a racing heart and headaches.
3. Hypovolemic POTS
- Cause: Low blood volume in the body, which can increase the symptoms of Postural Orthostatic Tachycardia Syndrome.
- Symptoms: Fatigue, fainting, and dizziness when standing. Patients often feel worse after exertion.
4. Secondary POTS
- Cause: This type is secondary to another condition, such as diabetes, Ehlers-Danlos syndrome, or multiple sclerosis.
- Symptoms: The underlying condition contributes to or worsens POTS symptoms. This includes rapid heartbeat, dizziness, and blood pooling.
Read More: Female CPR Training & What You Need to Know
What Are The Steps To Treat And Manage POTS?
Proper management and treatment of POTS helps improve the symptoms and enhance the quality of life. However, there is no one-size-fits-all treatment. Each patient’s case is unique and needs a personalized approach.
Here are few common steps that healthcare providers recommend-
- Increase Fluid and Salt Intake: Drinking 2-3 liters of water daily and increasing salt intake (unless contraindicated) helps maintain blood volume. It also reduces symptoms like dizziness and fainting.
- Physical Activity: Exercise focusing on strengthening the lower body and increasing cardiovascular endurance. This improves blood circulation and reduces POTS symptoms.
- Compression Garments: Wearing compression stockings or abdominal binders helps reduce blood pooling in the legs and improves circulation.
- Beta Blockers: Beta Blockers reduce the heart rate and help manage palpitations in some POTS patients.
- Fludrocortisone: A medication that helps retain salt and water to increase blood volume.
- Midodrine: This drug constricts blood vessels. It also prevents blood from pooling in the lower body.
- Ivabradine: Sometimes prescribed to manage an elevated heart rate.
- Frequent Small Meals: Eating smaller, more frequent meals can prevent post-meal drops in blood pressure.
- Avoiding Carbohydrate-heavy Meals: Large amounts of carbohydrates can increase blood pressure drops.
- Structured Exercise Program: Regular physical therapy can help improve tolerance to standing and exercise, slowly building endurance.
- Avoid Long Periods of Standing: Taking frequent breaks and sitting or lying down can help manage symptoms.
- Temperature Regulation: POTS patients may be sensitive to heat. It is important to stay cool with air conditioning, cooling vests, or cold drinks.
- Cognitive Behavioral Therapy (CBT): CBT and other forms of counseling can help manage anxiety, depression, or the emotional toll of living with a chronic illness.
- Regular Check-ups: Continuous monitoring and regular appointments with healthcare providers ensure that treatments are working and adjustments can be made as needed.
Read More: An Ultimate Guide to Cardiac Conduction System
What is the link between POTS and other underlying health conditions?
Many patients with POTS (Postural Orthostatic Tachycardia Syndrome) experience symptoms due to other medical conditions. This triggers the syndrome. Understanding the potential links between POTS offers insight into proper diagnosis and management strategies.
Ehlers-Danlos Syndrome (EDS): A connective tissue disorder that leads to joint hypermobility and skin elasticity, often seen in POTS patients.
Autoimmune Diseases: Conditions such as lupus, Sjögren’s syndrome, and celiac disease can coexist with POTS. This may indicate a possible autoimmune link.
Chronic Fatigue Syndrome (CFS/ME): Many people with CFS/ME also experience symptoms of POTS. This includes fatigue, dizziness, and heart rate irregularities.
Fibromyalgia: Patients with fibromyalgia often have overlapping symptoms with Postural Orthostatic Tachycardia Syndrome, such as widespread pain and autonomic dysfunction.
Mast Cell Activation Syndrome (MCAS): Some POTS patients also have MCAS. This causes allergic-like reactions and affects blood pressure and heart rate.
Diabetes: Nerve damage from diabetes, especially autonomic neuropathy, can contribute to the development of POTS symptoms.
Conclusion
Understanding the types of (POTS) Postural Orthostatic Tachycardia Syndrome, is important for proper diagnosis and management. Each type, whether it’s Neuropathic or Secondary, has its own challenges and symptoms. Recognizing these variations helps offer more precise treatment plans. This also helps patients understand their condition better. While living with POTS can be difficult, knowing which type is the first step toward improving symptoms and quality of life. With the right combination of lifestyle changes, medications, and support, managing POTS becomes a more attainable goal!