Transcutaneous pacing (TCP), also referred to as external pacing, is an essential emergency medical procedure applied to patients experiencing symptomatic bradycardia with a heart rate under 60 beats per minute. Did you know that it is the fastest way to achieve cardiac synchronization? Transcutaneous pacing capture utilizes external electrode pads placed on the chest to deliver an electric impulse that stimulates the heart muscle, causing contraction. This manages heart rhythm until definitive treatment resolves the underlying condition. Learn all about performing TCP with an approved ACLS training provider.
Master ACLS Now
Get ACLS certified with confidence
How does TCP work?
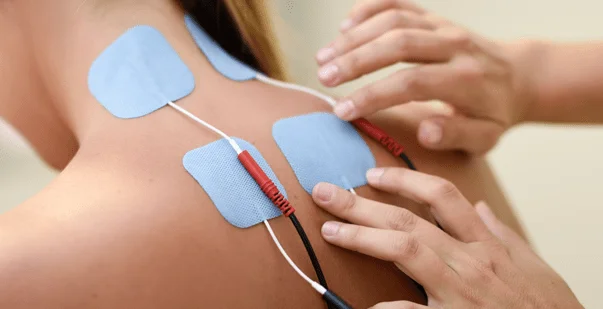
Transcutaneous pacing electrodes typically get placed in an anterior-posterior position on the upper right chest below the clavicle and on the left lateral side of the torso below the pectoral region. The external pacemaker device then delivers a small electrical charge between the pads to rhythmically stimulate the cardiac tissue to contract when the sinoatrial node fails to spark normal pulsations.
(Source: Nurse Key, Image Title: Transcutaneous Pacing)
TCP pulse generators can calibrate between 10 to 180 heartbeats per minute for customized rate responses based on patient age, typical resting heart rate parameters, and urgency of blood pressure deficits. The impulse must also have sufficient milliampere current to reach adequate ventricular tissue depth for “capture” – actually generating heart contractions rather than just pulsing electricity through the chest.
How is TCP capture achieved?
The pacing impulse results can be capture or non-capture. Capture means the external electrical stimulus successfully activates cardiac muscle fibers, causing an effective heart contraction. Clinicians visually confirm this by palpating a femoral pulse with the pacing spikes. The optimal sensing range falls between 2-10 milliamperes adjusted gradually while checking for palpable beats.
Non-capture means the external pacing spikes fail to trigger ventricular depolarization. This may result from inadequate current levels, poor pad electrode positioning, metabolic issues, or persistent arrhythmias. If the femoral pulse fails to generate above pacing outputs of 100 milliamperes, the TCP procedure gets aborted. At this point, the patient often receives medication infusions like dopamine or epinephrine to increase the force of contractions while the clinical team re-evaluates additional interventions like transvenous catheter placement or medication adjustments.
Master ACLS Now
Get ACLS certified with confidence
What is the essential utility of transcutaneous cardiac pacing?
Introduced first by Zoll and associates, Transcutaneous pacing, also known as external pacing, utilizes electrical impulses delivered from electrode pads positioned on the surface of the chest to stimulate cardiac muscle contractions. This safely manages unstable bradycardia until permanent pacemaker solutions or medications can establish an effective rhythm. For emergency teams, rapidly attaining consistent capture makes the difference.
What is mechanical capture in TCP?
Mechanical capture pacing refers to successfully triggering depolarization and subsequent pumping action of the heart chambers via applied electrical stimulation during TCP. Consistent capture then generates corresponding mechanical contractions as confirmed through palpable pulses and blood pressure waveform tracking.
Troubleshooting TCP capture requires gradually dialing electrical outputs in mA higher until physically transduced beats register during cardiac monitoring. Typically effective capture occurs between 50-100 mA for adults when pads are correctly anterior-posterior positioned. Failing capture above 100 mA prompts reevaluation of pad locations, alternative interventions, or medication use.
What is electrical capture in TCP?
The minimum threshold stimulating visible electrical activity on the ECG reading is electrical pacing capture. This may occur at lower mA outputs than mechanical capture depending on the presenting arrhythmia and metabolic state.
If electrical capture shows on the cardiac monitor but palpable pulses are not detected, then the pacing impulse successfully depolarizes the ventricle electrically but fails to release sufficient calcium ions to Generate forceful myocardial contractions. Here, you may need to use chronotropic medicines or higher mA output.
What are the TCP safety margin guidelines and how much of a safety margin for a transcutaneous pacemaker?
Ideally, transcutaneous pacing attempts to utilize the lowest milliampere current that establishes consistent mechanical capture for patient comfort and safety. However, clinicians also build in a margin between the threshold capture mA and subsequent outputs to account for shifts in electrodes or patient physiology.
A general safety margin for transcutaneous pacing for reliable capture gets set at least 5 mA higher than the initial lowest reading with successful beats. This ensures minor positional adjustments do not inadvertently lose capture mid-procedure while interventions take effect. Troubleshooting proceeds if rises occur.
What is the TCP utilization scope?
First responders and ED teams rely on transcutaneous pacing as a rapid, non-invasive intervention to stabilize bradycardia including heart blocks before cardiac catheterization laboratory or operating room transfer for permanent pacemaker implantation or medications take effect. Transcutaneous pacing capture offers a temporary bridge supporting blood pressure and vital organ perfusion.
Conclusion
Mastering urgent Transcutaneous pacing capture procedures with quality capture represents critical lifesaving skills for advanced cardiovascular emergency response teams. Correct electrode positioning, troubleshooting thresholds, and expert modifications make the difference until definitive heart rhythm solutions or alternative pharmacological options sufficiently recover native cardiac pacemaking abilities. If you are someone who has to deal with cardiac emergencies, you may want to consider taking a reputed ACLS course where you can learn all about transcutaneous pacing.