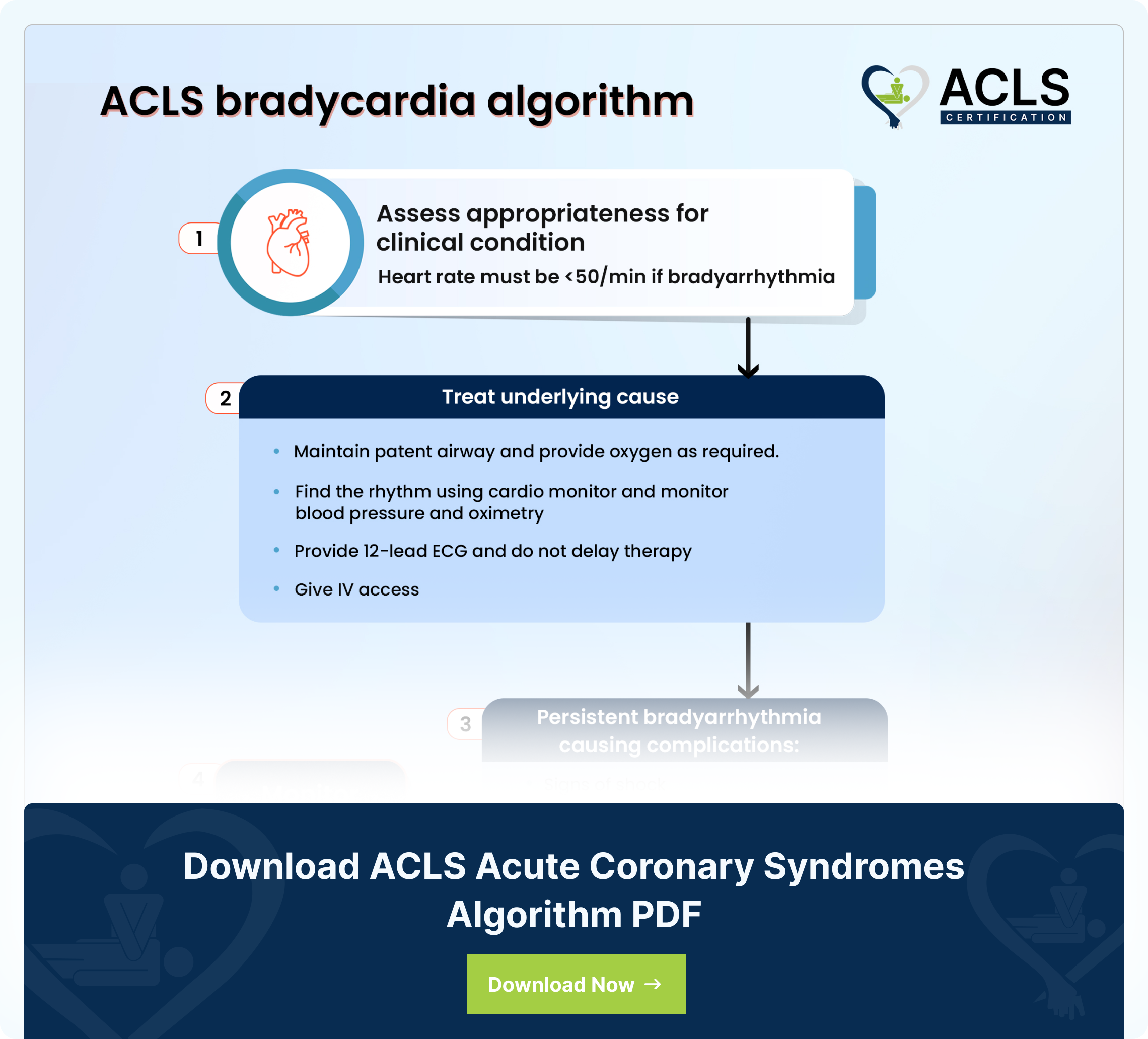
The ACLS (Advanced Cardiac Life Support) bradycardia algorithm helps manage patients with bradycardia. Bradycardia is a slow heartbeat condition, typically less than 50 beats per minute. The Bradycardia algorithm is a structured plan that involves checking the patient for symptoms while figuring out what might be causing the slow heart rate. It checks the airway clarity and keeps an eye on vital signs such as blood pressure, heart rhythm, and oxygen levels. Additionally, it also sets up IV access and offers appropriate treatments such as dopamine, epinephrine, and transcutaneous pacing whenever needed. Thus, it is a step-by-step approach that healthcare providers use to handle slow heart rates in a systematic manner.
Step by step analysis of flowchart
- Determine Appropriateness for Clinical Condition:
- Check the heart rate; if it is typically less than 50 beats per minute, it suggests bradyarrhythmia.
- Find and treat the underlying cause:
- Maintain a patent airway and assist breathing as necessary.
- Administer oxygen if the patient is short of breath.
- Use a cardio monitor to identify the rhythm, monitor blood pressure, and do oximetry.
- Establish intravenous (IV) access.
- Conduct a 12-lead ECG, if available, without delaying therapy.
- Evaluate for Complications of Persistent Bradyarrhythmia:
- Determine if persistent bradyarrhythmia is causing complications such as hypotension, acutely altered mental status, signs of shock, ischemic chest discomfort, or acute heart failure.
- If yes, then offer Atropine IV Dosing:
- Administer atropine as follows:
- First dose: Atropine 1mg
- Repeat every 3–5 minutes, up to a maximum of 3mg.
- If atropine is ineffective, consider further interventions.
- Administer atropine as follows:
- If no, then monitor and observe
- Interventions if Atropine is Ineffective:
</span >- Options include:
- Transcutaneous pacing
- Dopamine IV infusion: 5–20 mcg/kg per minute
- Epinephrine IV infusion: 2–10 mcg per minute
- Expert Consultation and Transvenous Pacing:
</span >- Seek expert consultation for additional guidance.
- Consider transvenous pacing if needed for a more definitive intervention.
Highlights of the ACLS bradycardia algorithm
- Assessment:
Determine Clinical Significance: Assess the clinical picture of the patient to decide if the bradycardia is producing complications. - Identification of Atropine Candidates:
Symptomatic Bradycardia: If the bradycardia shows symptoms such as altered mental status, chest pain, or hypotension, then treatment should be initiated. Unstable Patients: Patients who have evidence of bad perfusion, shock, and acute heart failure need urgent treatment. - Administration of Atropine:
Atropine Dosing: Administer atropine intravenously.
Initial dose: 0.5mg to 1mg. Do every 3-5 minutes, as much as 3 mg maximum dose.
Besides, in cases of insufficient effect or acquiring high-level heart block, take two pacings into account. - Transcutaneous Pacing:
Consider Transcutaneous Pacing: For patients who continue to be bradycardic in spite of atropine, external pacing may serve as a temporary option. - Expert Consultation:
Consult Cardiology or Pacing Expertise: Seek expert consultation, especially when the instability persists or correct pacing is not achieved. - Transvenous Pacing:
Consider Transvenous Pacing: Transvenous pacing becomes mandatory in the event of unresponsiveness to the atropine and external pacing, or when bradycardia persists with hemodynamic compromise due to the low output. - Monitoring and reassessment:
Continuous Monitoring: Continuously monitor the heart rate, blood pressure, pulse oximetry, responsiveness and overall clinical condition of the patient. - Reassessment:
Assess the need for an intervention as per the patient’s response and disposition to the clinical condition.
The highlights seem interesting? Download the ACLS bradycardia algorithm now.
Download ACLS bradycardia algorithm PDF
Sources
- Patterson, Kirsten K.; Olgin, Jeffrey E. (2022). "Bradyarrhythmias and Atrioventricular Block". Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier. pp. 1312–1320. ISBN 978-0-323-82467-5. https://en.wikipedia.org/wiki/ISBN_(identifier)
- "Arrhythmias and Conduction Disorders". The Merck Manuals: Online Medical Library. Merck Sharp and Dohme Corp. January 2008. Retrieved 16 December 2009. http://www.merck.com/mmpe/sec07/ch075/ch075a.html
- "What is Bradycardia?". WebMD. Retrieved 5 July 2021 https://www.webmd.com/heart-disease/atrial-fibrillation/bradycardia
- Bradyarrhythmias". The Lecturio Medical Concept Library. Retrieved 5 July 2021 https://www.lecturio.com/concepts/bradyarrhythmias/
- The single-dose administration of atropine was increased from 0.5 mg to 1 mg. Now give 1 mg for the first dose and then repeat every 3-5 minutes at the 1 mg dose. Also, the dopamine infusion rate for chemical pacing was changed to 5-20 mcg/kg/min https://acls-algorithms.com/acls-drugs/bradycardia/
All ACLS Algorithms
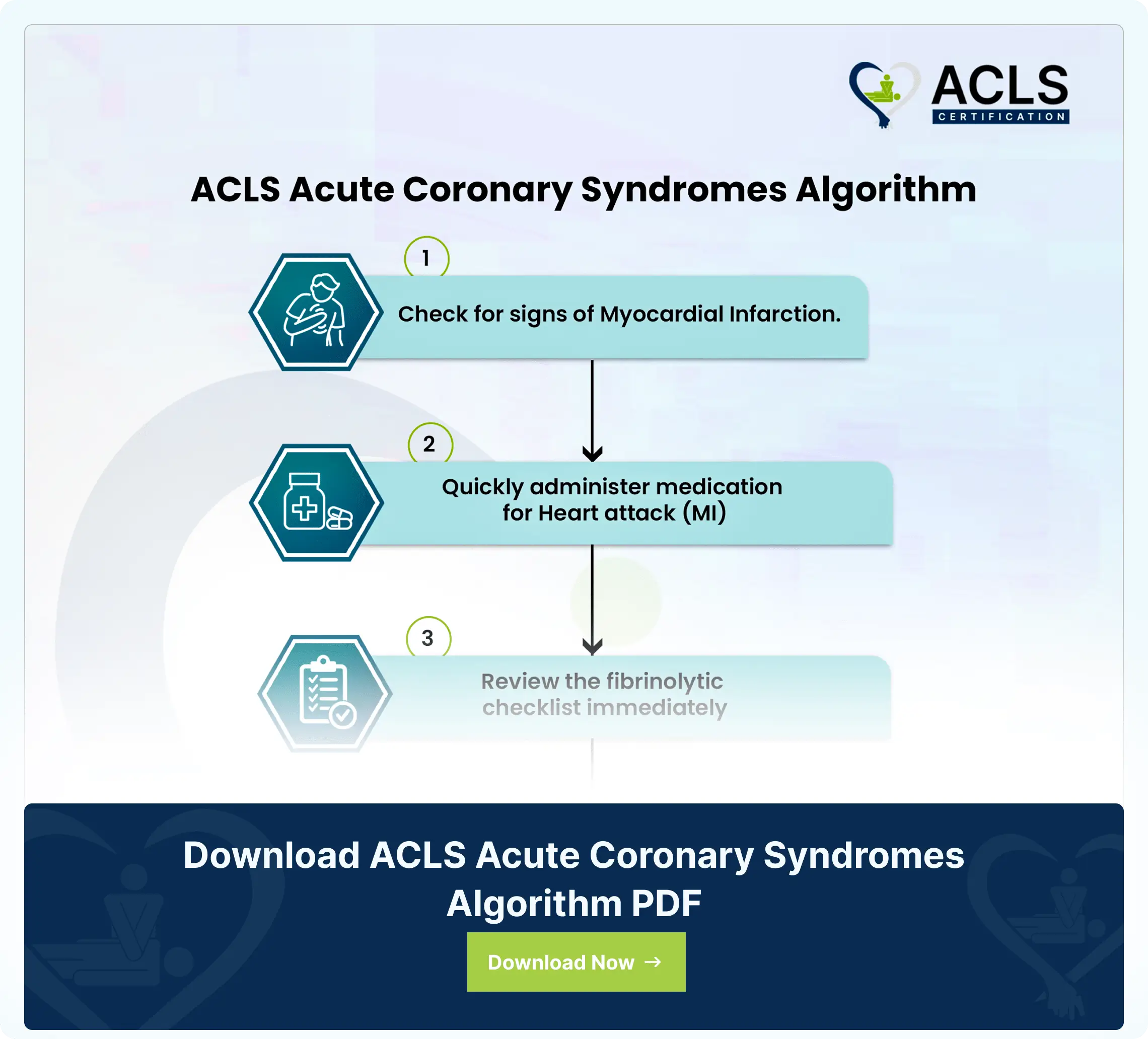
ACLS Acute Coronary Syndromes Algorithm
The ACLS Acute Coronary Syndromes Algorithm guides healthcare providers in the assessment, diagnosis, and treatment of patients with suspected or confirmed acute coronary syndromes
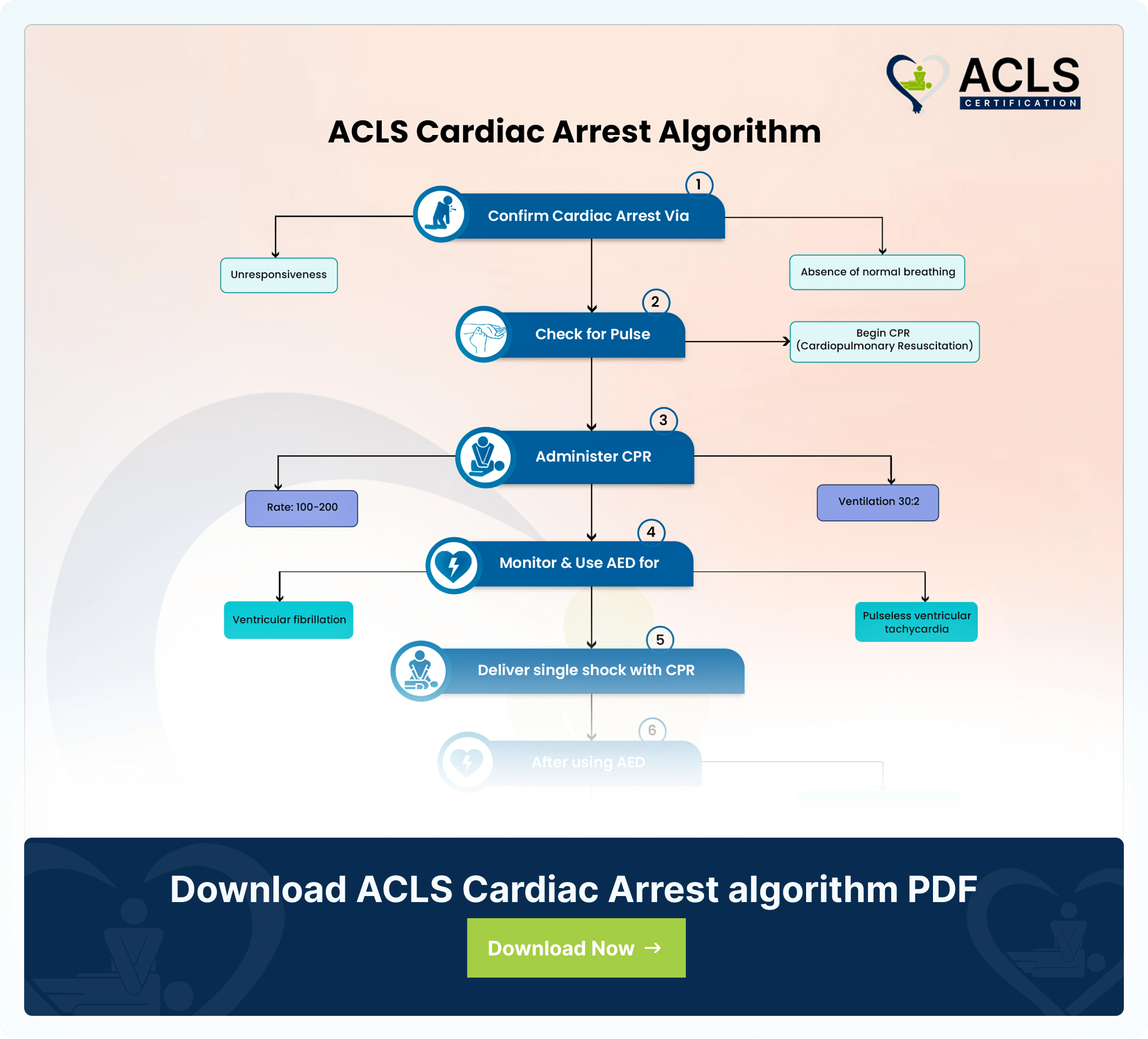
ACLS Cardiac Arrest Algorithm
The ACLS Cardiac Arrest Algorithm emphasizes CPR, defibrillation, drug therapy, and post-resuscitation care. It also highlights the importance of teamwork in optimizing outcomes during cardiac emergencies
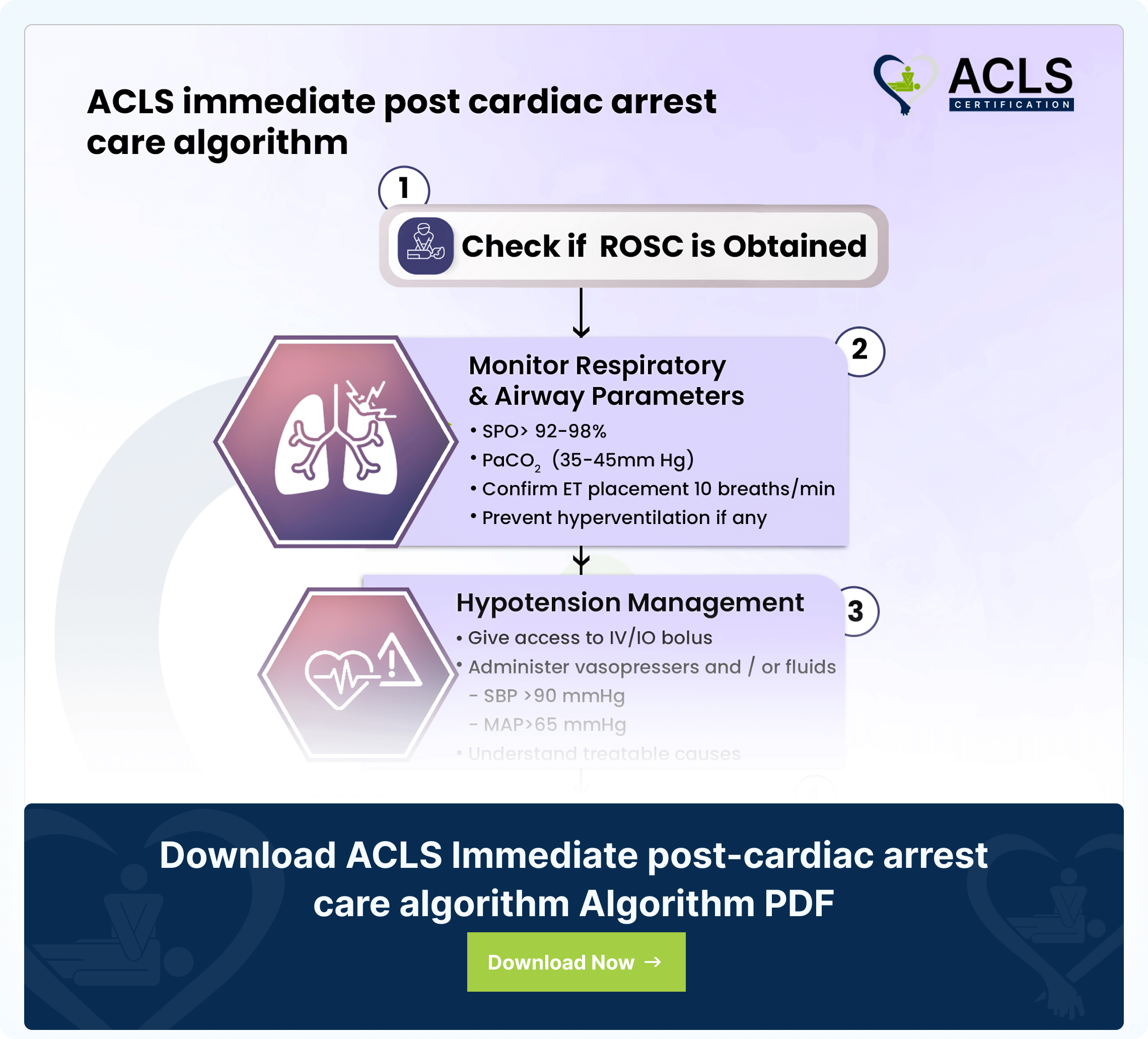
ACLS Immediate post-cardiac arrest care algorithm
The ACLS immediate post-cardiac arrest care algorithm guides critical interventions for patients post-resuscitation