Postural Orthostatic Tachycardia Syndrome (POTS) occurs when the body struggles to regulate blood flow, especially when transitioning from lying down to standing. When a person with POTS stands up, their heart rate increases significantly, often by more than 30 beats per minute or over 120 beats per minute. This causes dizziness, lightheadedness, or fainting. This guide walks you through the steps and tests used for POTS diagnosis, making it easier to recognize and manage this condition.
Master ACLS Now
Get ACLS certified with confidence
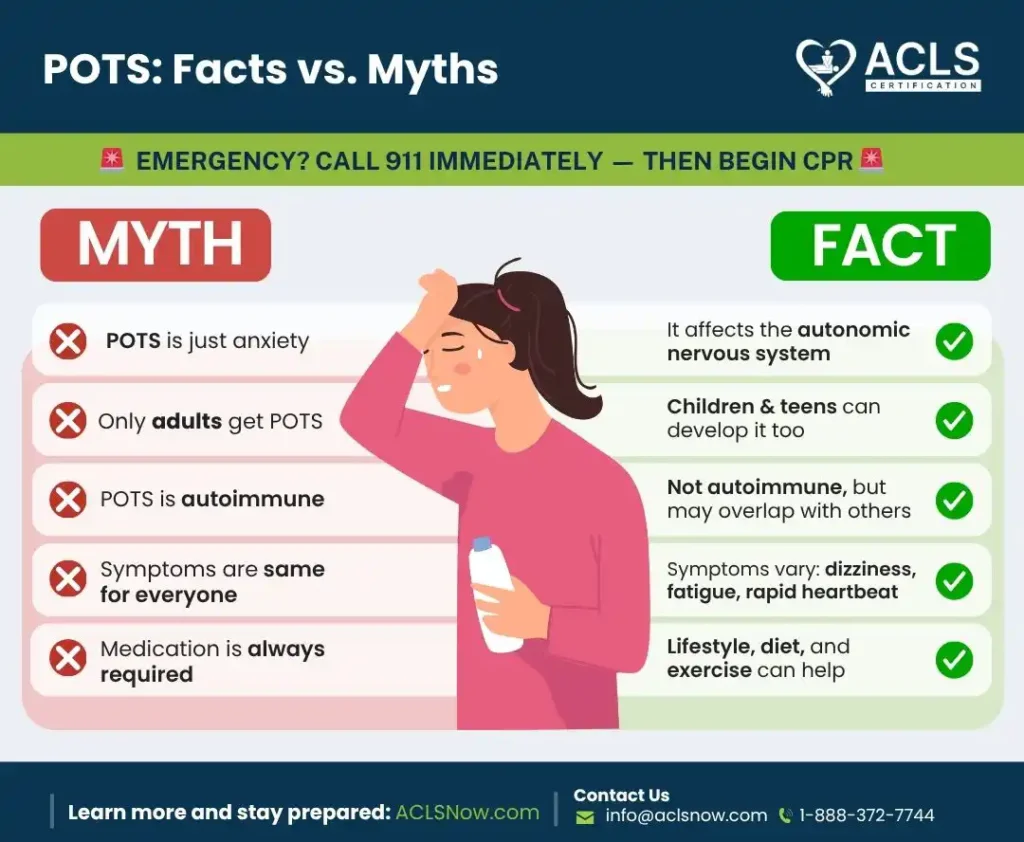
POTS: Facts vs. Myths
| MYTH ❌ | FACT ✅ |
| POTS is just anxiety | POTS affects the autonomic nervous system |
| Only adults get POTS | Children & teens can develop it too |
| POTS is autoimmune | Not autoimmune, but may overlap with other conditions |
| Symptoms are the same for everyone | Symptoms vary: dizziness, fatigue, rapid heartbeat |
| Medication is always required | Lifestyle, diet, and exercise can help manage symptoms |
Common Symptoms That Lead to Testing
Healthcare providers often explain how POTS is diagnosed by describing how the autonomic nervous system struggles to regulate blood flow. When someone has POTS, their symptoms can sometimes be mistaken for those of other conditions.
Knowing the common signs makes it easier to spot patterns and recommend further POTS testing methods. These symptoms often appear or worsen when standing and can significantly affect a person’s daily life. Let’s explore the most common ones.
Rapid Heartbeat (Tachycardia)
One major symptom of POTS is a noticeable increase in heart rate when standing. Patients may describe feeling like their heart is racing, even if they’re not doing anything strenuous. This happens because the autonomic nervous system struggles to regulate blood flow properly, causing the heart to compensate by pumping faster.
As a healthcare provider, observing this pattern in patients can be a reason to investigate further. A simple heart rate check while sitting and then standing can give you clues, but additional tests like the tilt table test confirm the diagnosis.
Dizziness and Lightheadedness
Patients with POTS often experience dizziness or feel lightheaded when they stand. Some even describe it as feeling like they might faint. This symptom can be unpredictable, making it frustrating for patients to manage in daily life.
You might encounter patients who avoid standing for long periods because they worry about feeling faint. When you hear such concerns, it’s a good reason to consider testing for POTS. Documenting how often these episodes happen and any triggers they mention can help guide diagnosis.
Fatigue and Brain Fog
Extreme tiredness and difficulty focusing are also common in POTS. Patients may describe feeling drained even after basic activities and many struggles with concentration or memory, often called “brain fog.”
It can be challenging to attribute these symptoms directly to POTS without knowing the context. If a patient reports fatigue that worsens with standing or brain fog that interferes with their routine, it’s worth exploring further.
Hidden or Overlooked Symptoms
Not all POTS symptoms are obvious, which can delay diagnosis. Some of the lesser-known symptoms are:
Nausea After Standing
Some individuals with POTS feel queasy or experience nausea after standing for less time. This happens because blood flow shifts away from the digestive system, making it difficult to process food normally. Thus, nausea may limit daily routines.
Temperature Regulation Issues
Feeling uncomfortably hot even in mild weather or unusually cold in warm rooms. It may indicate an underlying autonomic dysfunction. This is because the body affected by POTS may struggle to regulate temperature properly.
Shakiness or Tremors
Some people experience shakiness or internal tremors when standing. This is caused by poor blood circulation. Patients may describe it as “feeling jittery” or having hands that shake, easily mistaken for anxiety.
Initial Steps in Diagnosis
The initial POTS diagnostic criteria involve gathering a detailed picture of the patient’s health and symptoms before conducting specialized tests. These early evaluations help determine if further testing is needed and can rule out other potential causes. These steps are as follows:
Patient History and Symptom Discussion
A doctor who diagnoses POTS will review your symptoms and medical history to help make the right diagnosis. This includes asking when symptoms began, their frequency, and what triggers or worsens them. Many online POTS symptoms ask about specific triggers, such as heat or dehydration, to assess the likelihood of the condition.
As someone preparing for an ACLS course, you’ll learn to listen carefully and ask open-ended questions. For example, asking patients how long they can stand before symptoms appear can provide valuable information.
Family History of Autoimmune Conditions
As POTS often overlaps with other conditions, providers may ask about family history. Disorders such as Ehlers-Danlos syndrome or elastic skin, which affects joints and skin, lupus, or autoimmune thyroid disease, can increase the probability of autonomic dysfunction. Documenting this information can help build a more complete diagnostic picture and guide an effective treatment plan.
Physical Examination
While a POTS quiz is a good start, a doctor’s diagnosis is needed for confirmation. Checking heart rate and blood pressure while the patient is lying down, sitting, and standing can reveal patterns associated with POTS. For example, a significant increase in heart rate upon standing is a key indicator.
This step doesn’t require advanced equipment and can often be done during an office visit. Observing changes in vital signs during posture shifts helps you identify potential autonomic issues. Noticing these early trends can guide you toward the next steps in confirming a diagnosis.
Lifestyle and Health Factors
It’s also useful to consider factors like diet, hydration, and sleep habits. Patients with POTS often report dehydration or issues with salt intake, which can influence symptoms. Discussing these areas helps identify patterns or triggers. You might need a POTS blood test to help your doctor understand your overall health.
This information allows you, as a healthcare provider, to recommend simple adjustments while waiting for further test results. Small changes, such as drinking more fluids or increasing salt intake (if appropriate), can sometimes provide immediate relief and support the diagnostic process.
Misdiagnosis Alert
Many patients with POTS are initially told they have anxiety, panic disorder, or chronic fatigue syndrome. As the symptoms overlap, they can delay proper diagnosis and therapy. Recognizing these red flags early ensures patients are directed toward appropriate testing.
Read More: POTS Diet Plan: Best Foods & Foods to Avoid
Diagnostic Tests
Diagnosing POTS involves observing how the body reacts to changes in posture, particularly standing. These POTS tests focus on heart rate and blood pressure and how they change with movement. Let’s explore the most common POTS syndrome tests.
Tilt Table Test
One common way to answer how POTS is diagnosed is through the tilt table test, which tracks changes in heart rate and blood pressure. Before the tilt test for POTS, you may be asked to fast for a few hours to ensure accurate results. During this test, the patient lies on a table that tilts upward to mimic standing. The table moves while the patient’s heart rate and blood pressure are closely monitored.
You may notice that patients with POTS experience a sharp increase in heart rate without a significant drop in blood pressure. This reaction helps differentiate POTS from other conditions like orthostatic hypotension. The tilt table test POTS is often done in a controlled environment to keep the patient safe while gathering accurate data.
Active Stand Test
If you’re unsure how to test for POTS, starting with an active stand test can provide useful preliminary data. This test is a simpler alternative to the tilt table test. Here, the patient starts in a lying position and then stands up while their heart rate and blood pressure are recorded over a set period.
As a healthcare provider, this test is something you might perform in a clinic without specialized equipment. It allows you to observe how a patient’s heart rate responds to standing in real time. While it’s less precise than the tilt table test, it can still offer valuable insights when POTS is suspected.
Blood Volume Testing
Since low circulating blood volume (hypovolemia) is common in POTS, doctors may order blood volume testing. In this test, the plasma and red blood cell volume are assessed to see if the body is holding enough fluid. Identifying hypovolemia helps guide treatment strategies such as increased fluid intake, salt supplementation, or medications.
QSART (Sweat Test)
The Quantitative Sudomotor Axon Reflex Test (QSART) checks how well nerves control sweating, which is part of the autonomic nervous system. In this test, mild electrical stimulation is used to measure sweat at different sites on the body. Most of the POTS patients are affected by impaired autonomic function, and an abnormal QSART result can support proper diagnosis.
Holter or ECG Monitoring
Because heart rhythm issues can overlap with POTS symptoms, physicians sometimes recommend continuous heart monitoring. A Holter monitor records heart activity over 24 to 48 hours, whereas longer-term event monitors may track irregular rhythms for weeks. This helps rule out arrhythmias (irregular heartbeats). It also ensures that rapid heart rate episodes are due to POTS from other heart conditions.
Additional POTS Testing Methods
Other tests might be used to rule out conditions with similar symptoms or to understand the underlying causes of POTS. When you get POTS blood test results, your doctor may check for issues like anemia or thyroid problems. Neurological exams may assess nerve function, and cardiac monitoring (like a Holter monitor) can track heart activity over days.
How is POTS Treated?
Most people see progress through a combination of behavioral changes, lifestyle adjustments, and, in some cases, medications. Here’s a closer look at the main strategies.
Increase Sodium and Fluid Intake
One common reason for POTS symptoms is low circulating blood volume. Increasing sodium in your diet helps the body retain more fluids, which boosts blood volume and reduces symptoms like lightheadedness.
For many with POTS, the recommended sodium intake is up to three times higher than the standard guideline of 2,300 milligrams per day. Salty foods like tomato juice, broth, pickles, and olives are good options. High-sodium electrolyte drinks or salt tablets can also be effective. For instance, starting your day with a glass of tomato juice or adding a salt tablet to your lunch can make a noticeable difference.
Use Compression Garments
Compression garments help prevent blood from pooling in the lower parts of the body, especially when standing. They push blood into deeper veins, improving circulation and reducing symptoms.
Options include knee-high socks, calf sleeves, leggings, or bike shorts. Studies show that combining an abdominal binder with compression socks can provide significant relief. Choosing the right garment often depends on your lifestyle and comfort. For example, compression bike shorts paired with socks are a popular choice for active individuals.
Gradual Exercise Program
Exercise is a cornerstone of POTS treatment, but it must be approached carefully. Many people with POTS struggle with fatigue and dizziness during workouts, so it is effective to start with low-impact exercises and gradually increase intensity.
Read More: What Are the Best Hydrating Foods for Patients With POTS?
Getting Started with POTS Diagnosis
Getting a POTS diagnosis can take time, but learning about the steps makes it easier. Tests like the tilt table test or blood work are used to figure out what’s causing the symptoms. When you understand the process of POTS diagnosis, it can make you feel more prepared for discussion with your doctor. With the right tests and support, you can find answers and start managing your condition. Taking the time to explore your symptoms can lead to better results.
FAQs
Why does it take years to get a POTS diagnosis?
The symptoms of POTS often mimic other conditions. It is still not widely recognized, so patients may see multiple doctors before getting a correct diagnosis.
Can POTS be mistaken for anxiety or panic attacks?
Yes. Rapid heart rate, dizziness, and fatigue can resemble anxiety or panic. These symptoms can delay proper diagnosis.
What is the gold standard test for diagnosing POTS?
The tilt table test is the most reliable test to confirm POTS. It measures the heart rate and blood pressure changes while standing.
Do children and teens get POTS?
Yes. POTS can affect children, teens, and adults, often becoming noticeable during adolescence.
Can POTS go away with treatment?
Symptoms can improve with lifestyle changes, medication, and gradual exercise. But, in some patients, the symptoms may be persistent for a long time.
Is POTS an autoimmune condition?
Not really. POTS is primarily an autonomic nervous system disorder. But it may sometimes occur alongside other autoimmune conditions, such as lupus, Ehlers-Danlos, etc. in some patients.
References:
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/postural-orthostatic-tachycardia-syndrome-pots#:~:text=POTS%20diagnosis%20can%20be%20complicated,nerves%20responsible%20for%20regulating%20sweating.
- https://www.health.harvard.edu/blog/pots-diagnosing-and-treating-this-dizzying-syndrome-202110062611
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8920526/