In the domain of Advanced Cardiovascular Life Support (ACLS), success hinges on collaborative efforts. It emphasizes the collective contributions of each team member, capitalizing on their individual strengths. From cohesive communication to mutual support and respect, effective teamwork serves as the cornerstone of team dynamics in ACLS scenarios. This blog talks about and looks into the very basics of team dynamics within ACLS.
We will be exploring the human elements that go way beyond just the resuscitation efforts from just a mere protocol to life-saving collaboration.
Master ACLS Now
Get ACLS certified with confidence
Why is Effective Teamwork Crucial in ACLS?
Effective teamwork in Advanced Cardiovascular Life Support (ACLS) scenarios is imperative because it is a space where rapid and coordinated actions are needed for better patient outcomes. Here’s how team dynamics contribute to successful ACLS interventions:
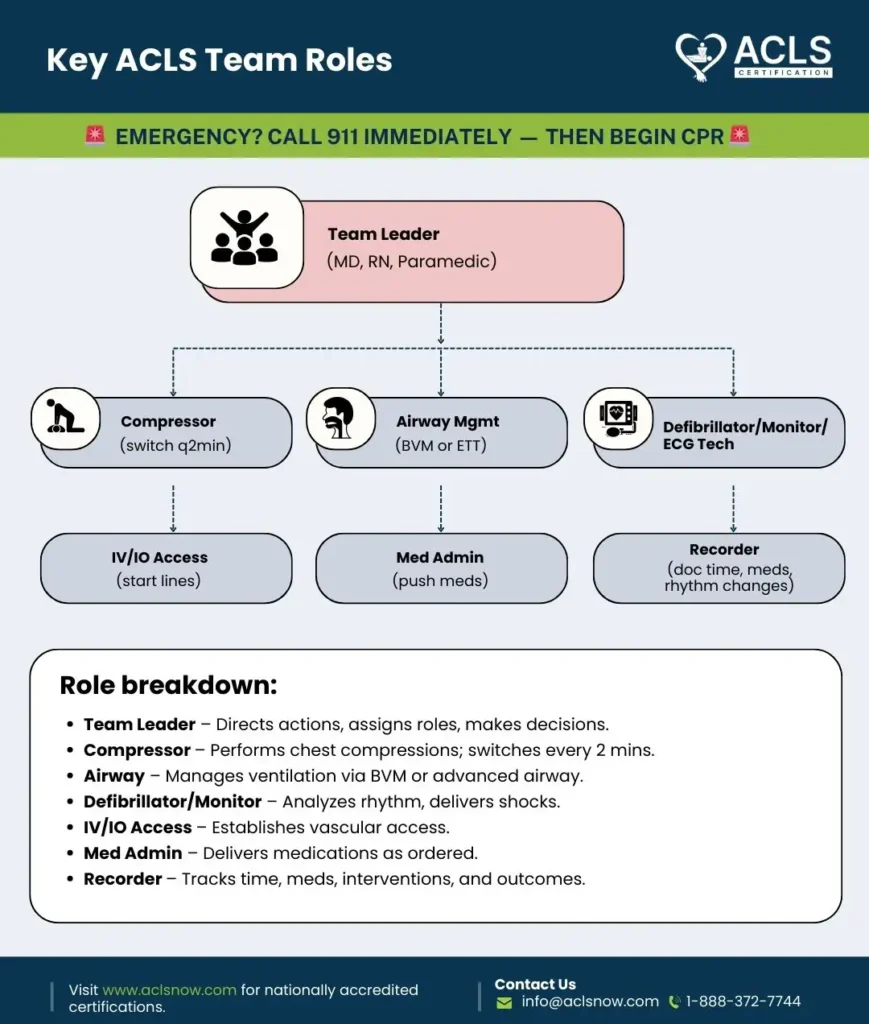
Clear Roles and Responsibilities:
Defined roles ensure that each team member knows their tasks. So be it from team leaders to compressors and airway managers. This clarity prevents any kind of confusion during high-stress situations.
Communication Strategies:
Clear and concise communication, including closed-loop communication and briefings, facilitates the exchange of critical information among team members. This helps that everyone is informed and aligned and so it reduces the risk of errors.
Mutual Respect and Constructive Intervention:
A culture of mutual respect leads to an environment where team members feel comfortable when they are voicing concerns and providing constructive feedback. This promotes collaboration and enables rapid adaptation to circumstances very easily.
Adaptability and Flexibility:
Team members must remain adaptable and flexible in dynamic ACLS scenarios, ready to adjust strategies based on patient response and evolving conditions. This ensures the team can take care of any unexpected challenges.
Read More: Acls discount code
What Communication Strategies Enhance ACLS Team Performance?
Here are several communication strategies that can improve ACLS team performance:
Clear Roles and Responsibilities:
This means that each team member understands their role and responsibilities during ACLS interventions. They clearly define who is responsible for tasks such as airway management, chest compressions, medication administration, and documentation.
Closed-loop Communication:
This incorporates an encouragement of a communication style where information is relayed, acknowledged, and confirmed. This ensures that messages are received very accurately and understood by all team members. For example, when a team member gives an instruction or report, others should confirm receipt and understanding by repeating back the information.
Standardized Communication Protocols:
Here it talks of standardized communication protocols such as SBAR (Situation, Background, Assessment, Recommendation) to allow very clear and concise communication among team members. This format helps to ensure that critical information is conveyed properly, during handoffs and transitions of care particularly.
Team Huddles and Briefings:
Now this involves pre-procedure huddles and briefings to review the patient’s condition. This is actually done to establish goals, assign roles, and address any concerns or questions. These briefings help to synchronize team efforts and also make sure that everyone is on the same page before they even begin ACLS interventions.
Closed-loop Debriefings:
After the ACLS interventions, conduct closed-loop communication CPR, debriefings to review the team’s performance, identify strengths and areas for improvement, and discuss lessons learned. You must encourage open communication during debriefings and emphasize constructive feedback to create a culture of regular improvement.
Use of Clear and Concise Language:
In high-stress situations, communication can become fragmented or misunderstood so it is important to use clear language to convey critical information effectively. Also, avoiding medical jargon or ambiguous terminology that may lead to confusion is also important.
Master ACLS Now
Get ACLS certified with confidence
How Can ACLS Teams Optimize Their Performance?
Optimizing ACLS (Advanced Cardiovascular Life Support) team performance requires a combination of effective teamwork, preparation, training, and adherence to evidence-based practices. Here are several key strategies for ACLS teams to optimize their performance:
Regular Training and Simulation:
Conduct regular ACLS training sessions and simulations to reinforce team dynamics, roles, and skills. Simulation-based training allows teams to practice managing various emergency scenarios in a controlled environment, helping to improve coordination and decision-making under pressure.
Teamwork and Communication:
Emphasize the importance of teamwork and communication skills during ACLS interventions. Encourage clear communication, closed-loop feedback, and a shared understanding of roles and responsibilities among team members.
Adherence to Algorithms and Protocols:
Follow established ACLS algorithms and protocols based on current guidelines and best practices. Standardized protocols provide a framework for systematic assessment and treatment, helping to ensure consistency and effectiveness in patient care.
Equipment Familiarization and Maintenance:
Ensure that ACLS team members are familiar with the use and maintenance of essential equipment such as defibrillators, airway devices, and medications. Regular equipment checks and maintenance help to prevent delays or errors during emergency interventions.
Documentation and Follow-up:
Ensure accurate and timely documentation of ACLS interventions, including patient assessment findings, treatments administered, and response to therapy. Follow up with appropriate post-resuscitation care and monitoring to optimize patient recovery and prevent recurrence of cardiac events.
Conclusion
Team dynamics in ACLS and its success depend on teamwork and communication. Through regular training and role clarity, teams can optimize performance when faced with life-or-death scenarios. So adaptability and supporting one another encourage resilience and continuous improvement. Behind every successful resuscitation lies a team of healthcare heroes, united in their mission to save lives.
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9373058/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8562429/
- https://promedcert.com/blog/5-elements-of-effective-team-dynamics-in-acls/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5509566/
- https://www.ncbi.nlm.nih.gov/books/NBK549899/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963226/