Acute Myocardial Infarction or AMI is a serious medical condition which is popularly known as the Heart Attack. It is a critical medical condition that happens when blood flow to the vital organs stop, leading to muscle damage. The blockage is basically due to the buildup of plaque in the arteries. The constant buildup of plaque often ruptures the arteries and forms a clot. Prompt diagnosis and treatment is crucial. One of the most vital tools in diagnosing AMI is through ECG’s Electrocardiograms. ECG provides a real time snapshot of the heart that helps doctors assess the electrical activity of the heart.
This blog will elaborate on the role of ECG to diagnose Acute Myocardial Infarction (AMI). We will also be exploring the key patterns and changes that denote an ongoing heart attack. Along with that we will also explore classic ECG findings associated with AMI (Acute Myocardial Infarction).
Master ACLS Now
Get ACLS certified with confidence
What are the signs of myocardial infarction through ECG?
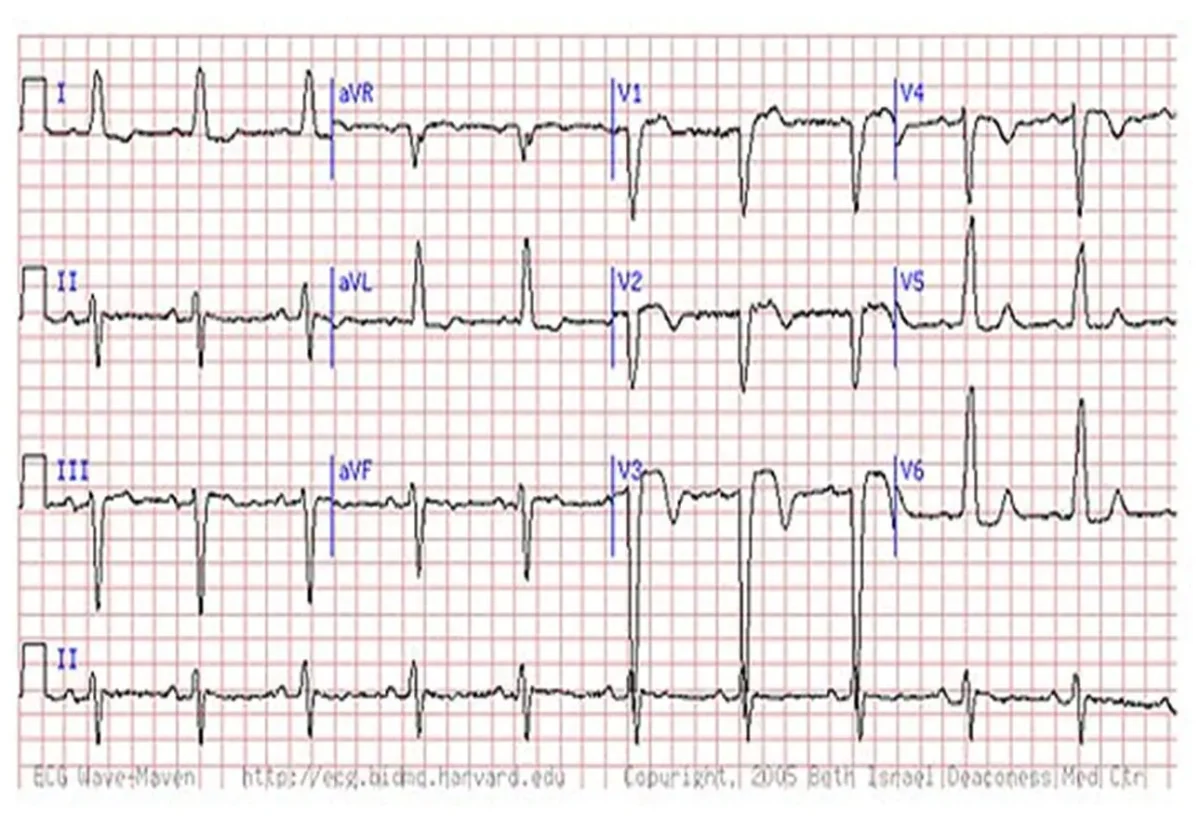
Electrocardiograms (ECGs) are critical in diagnosing acute myocardial infarction (AMI). It provides real-time insights into the heart’s electrical activity. Recognizing the signs of AMI on an ECG is essential for timely and effective treatment. Here are the key ECG signs indicative of myocardial infarction:
- ST-Segment Elevation: This is the hallmark of an acute myocardial infarction. It indicates severe ischemia and injury to the heart muscle.
- T-Wave Inversion: This can be an early sign of ischemia or a developing myocardial infarction.
- Pathological Q Waves: These suggest the presence of necrosis and are typically seen later in the course of an infarction.
- ST-Segment Depression: Often seen in cases of subendocardial ischemia or non-ST-elevation myocardial infarction (NSTEMI).
- New Left Bundle Branch Block (LBBB): This can mask the signs of myocardial infarction and is considered a potential indicator of AMI when seen in the right clinical context.
Read More: Ventricular Fibrillation: Causes, Symptoms, and Treatment
What are the signs and symptoms of AMI(Acute Myocardial Infarction)?
Acute Myocardial Infarction (AMI), commonly known as a heart attack, occurs when blood flow to a part of the heart is suddenly blocked, leading to heart muscle damage. Recognizing the signs and symptoms of AMI is crucial for prompt medical intervention and improving patient outcomes. Here are the common signs and symptoms of acute myocardial infarction:
- Chest Pain or Discomfort: Often described as pressure, squeezing, fullness, or pain in the center or left side of the chest, which can last for more than a few minutes or come and go.
- Upper Body Pain: Discomfort or pain may spread to the shoulders, arms, back, neck, jaw, or stomach.
- Shortness of Breath: This can occur with or without chest discomfort and may be more pronounced during physical activity or at rest.
- Sweating: Profuse sweating, often described as a cold sweat.
- Nausea and Vomiting: Some individuals may experience nausea or vomiting, which can be mistaken for other conditions such as indigestion.
- Lightheadedness or Dizziness: Feeling faint or lightheaded can be a sign of reduced blood flow to the brain.
- Fatigue: Unusual tiredness or weakness, especially in women, which may precede other symptoms by days or weeks.
Recognizing these symptoms early and seeking immediate medical attention can significantly improve the prognosis for individuals experiencing an acute myocardial infarction.
Read More: What Are The Shockable Rhythms
What happens if AMI(Acute Myocardial Infarctions) are not diagnosed promptly?
Acute Myocardial Infarctions (AMIs), or heart attacks, require immediate medical attention to prevent severe complications and improve patient survival rates. If AMIs are not diagnosed and treated promptly, the consequences can be dire. Here are the potential outcomes of delayed diagnosis and treatment of AMI:
- Increased Heart Muscle Damage: Prolonged lack of blood flow leads to more extensive damage to the heart muscle, which can impair its ability to pump effectively.
- Heart Failure: Significant loss of functional heart muscle can lead to heart failure, where the heart cannot pump enough blood to meet the body’s needs.
- Cardiac Arrest: The heart may stop beating suddenly due to severe arrhythmias, such as ventricular fibrillation or ventricular tachycardia, which can be fatal without immediate intervention.
- Cardiogenic Shock: A severe complication where the heart is unable to supply enough blood to the organs, leading to multiple organ failure and high mortality rates.
- Chronic Heart Conditions: Survivors of untreated or poorly managed AMI may develop chronic conditions like angina (chest pain), arrhythmias (irregular heartbeats), or persistent heart failure.
- Increased Mortality: The risk of death significantly increases with delayed treatment due to the progression of heart damage and the likelihood of complications.
Conclusion
Electrocardiograms are vital tools when it comes to diagnosing Acute Myocardial Infarction (AMI). It is important to understand the key changes in ECG, like st segment elevation in ecg. Prompt recognition of such signs leads to earliest intervention, increasing the chances of recovery. So it is extremely important for all healthcare providers to continually learn and achieve precision in ecg interpretation.