Atropine Sulfate is an FDA approved drug that carries anti-sialagogue/ anti-vagal effect. It is a critical medication used in the Advanced Cardiovascular Life Support (ACLS) algorithm. An ideal atropine ACLS dose is used to treat symptomatic bradycardia. Bradycardia is a condition in which a patient has abnormally slow heart rate, leading to compromised organ perfusion. Understanding the correct dosage to administer atropine sulfate helps manage life-threatening complications.
In this blog we will discuss the specifics of atropine sulfate as a crucial ACLS drug. We will also explore its pharmacological actions, clinical indications and important considerations. Read along and learn to confidently use atropine sulfate in emergencies.
Master ACLS Now
Get ACLS certified with confidence
What are the pharmacological actions of atropine in ACLS?
Used for its potent pharmacological effects, atropine sulfate manages symptomatic bradycardia. This drug works by blocking the parasympathetic influences on the heart. Below mentioned are the main pharmacological actions of atropine-
- Inhibition of Parasympathetic Activity: Atropine is an anticholinergic agent that blocks the action of acetylcholine on muscarinic receptors in the heart. This inhibition reduces vagal tone, which is responsible for slowing down the heart rate.
- Increased Heart Rate: By blocking the parasympathetic effects, Atropine allows the sympathetic nervous system to dominate, resulting in an increased heart rate (positive chronotropic effect). This can help improve cardiac output and organ perfusion in patients with bradycardia.
- Enhanced Atrioventricular (AV) Conduction: Atropine facilitates the conduction of electrical impulses through the AV node, which can help counteract AV block and improve the synchronization of atrial and ventricular contractions.
- Reduction of Secretions: Atropine decreases salivary and respiratory secretions, which can be beneficial during intubation and other airway management procedures in emergency settings.
- Bronchodilation: Atropine can cause mild bronchodilation by relaxing smooth muscles in the airways, which may aid in improving ventilation in patients experiencing bronchospasm or airway obstruction.
Read More: ACLS Certification in New Mexico
What are the clinical indications of atropine use in ACLS?
Primarily used to counteract the effects of excessive vagal stimulation, atropine saves lives where bradycardia and other related conditions threaten patient stability. Below are the key clinical indications for the use of Atropine in ACLS:
Symptomatic Bradycardia: Atropine is the first-line treatment for symptomatic bradycardia. It is characterized by a heart rate that is too slow to maintain adequate cardiac output. This leads to symptoms of hypotension, altered mental status, chest pain, or signs of shock.
Atrioventricular (AV) Block: Atropine is indicated for certain types of AV block, particularly first-degree and second-degree Type I (Wenckebach) AV block, where it can help improve conduction through the AV node and stabilize the heart rhythm.
Organophosphate Poisoning: Atropine is used as an antidote in cases of organophosphate poisoning. This can cause excessive cholinergic activity, leading to severe bradycardia and other parasympathetic symptoms.
Premedication for Intubation: In some cases, Atropine is administered as a pre-medication before intubation to reduce secretions and prevent reflex bradycardia associated with airway manipulation, particularly in pediatric patients.
Asystole and Pulseless Electrical Activity (PEA): Although not a primary treatment, Atropine may be considered in cases of asystole or PEA, particularly if there is a suspected vagal-mediated component contributing to the arrest.
Atropine in ACLS: Important Considerations To Keep In Mind
Atropine’s pharmacological properties are life saving, but it is equally important to keep the considerations in mind to make the most out of this drug. Here are the potential side effects and key considerations to keep in mind:
Correct Dosing
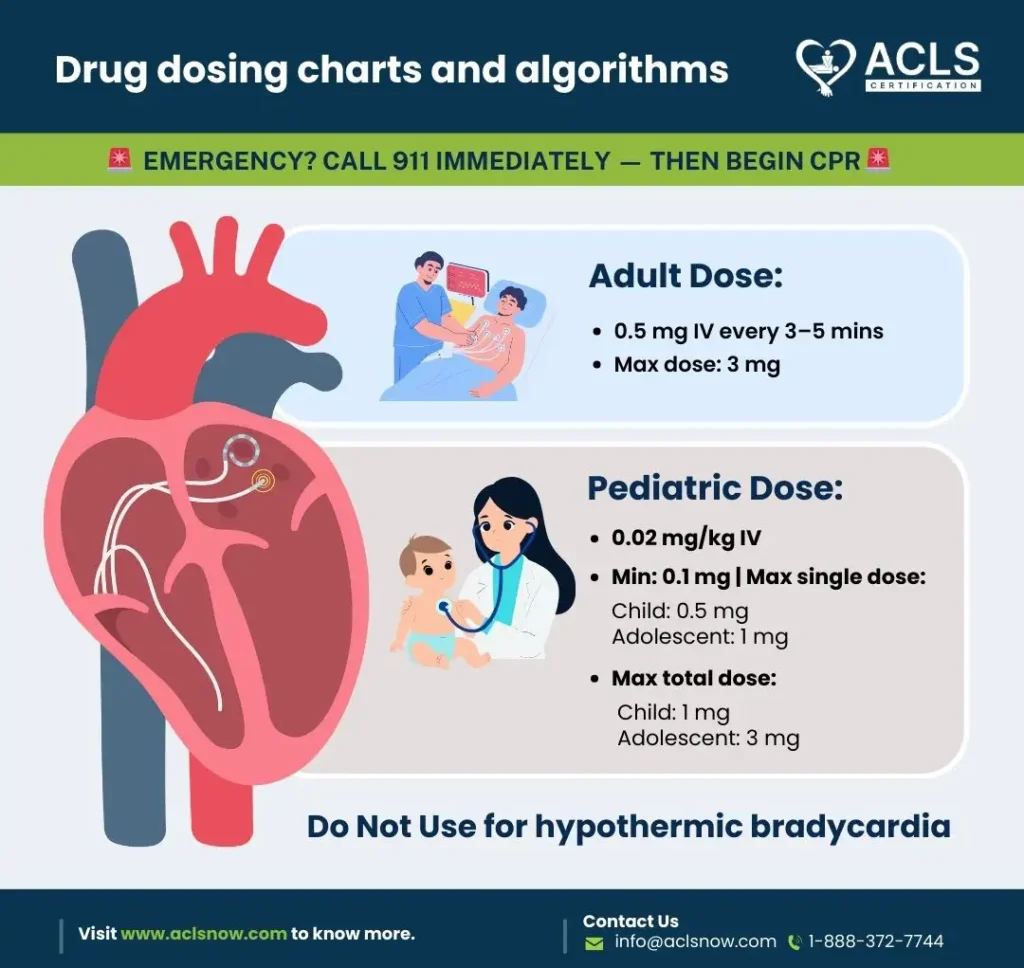
- Recommended Dose: The typical dose of Atropine for symptomatic bradycardia in adults is 1 mg administered intravenously. This dose can be repeated every 3-5 minutes as needed, with a maximum total dose of 3 mg.
- Pediatric Dosing: For pediatric patients, the recommended dose is 0.02 mg/kg IV/IO, with a minimum dose of 0.1 mg and a maximum single dose of 0.5 mg for children and 1 mg for adolescents. The maximum total dose is 1 mg for children and 2 mg for adolescents.
Monitoring and Response
- Patient Monitoring: Continuous ECG monitoring is essential to assess the patient’s heart rate and rhythm, ensuring that Atropine is having the desired effect.
- Response Time: Atropine typically acts within minutes. If there is no improvement after the maximum dose, consider alternative treatments.
Potential Side Effects
- Tachycardia: Atropine can cause an excessively rapid heart rate, which may be problematic, particularly in patients with ischemic heart disease.
- Dry Mouth and Blurred Vision: Anticholinergic side effects such as dry mouth, blurred vision, and urinary retention are common but typically not life-threatening in the acute setting.
Contraindications and Cautions
- Contraindications: Atropine is contraindicated in patients with hypersensitivity to the drug, and it should be used cautiously in those with glaucoma, obstructive uropathy, or myasthenia gravis.
- Heart Transplant Patients: Atropine may be ineffective in patients who have undergone heart transplantation due to denervation of the vagus nerve in the transplanted heart.
Special Situations
- Organophosphate Poisoning: Higher doses of Atropine may be necessary for patients with organophosphate poisoning due to severe cholinergic overstimulation.
- Environmental Factors: Ensure that the storage and handling of Atropine are according to guidelines, as extreme temperatures can affect its potency.
Read More: ACLS vs. Emergency Medical Technician
Conclusion
The atropine ACLS dose manages symptomatic bradycardia and certain types of AV blocks. Understanding the right dosage, clinical indications and considerations are crucial for effective results. Atropine is lifesaving in fatal emergencies, but healthcare professionals should be equally invested in potential alternative treatments. Staying updated and aware of new ACLS guidelines ensure patients the best possible care that adheres to industry standards. Don’t forget to equally focus on ACLS courses to understand more about important ACLS drugs and their contribution in critical cardiac emergencies.