In advanced life support care for cardiac arrest cases, you should focus on regular monitoring of the patient’s condition to stabilize and sustain their survival rate. One parameter that you need to monitor while administering cardiopulmonary resuscitation is EtCO2 levels.
EtCO2 monitoring can tell you a lot about what may be going on with the victims, from the continuous feedback on CPR quality to the confirmation of airway placement. The technique with accurate determinants will provide insights into the effectiveness of chest compressions in CPR and aid in optimizing your resuscitation outcomes. Now, what is the main determinant of EtCO2 during CPR? Read on to find out!
Master ACLS Now
Get ACLS certified with confidence
What Does EtCO2 Stand for?
EtCO2 stands for end-tidal carbon dioxide, which refers to the level of carbon dioxide (CO2) measured at the end of an exhaled breath. This measurement provides real-time insights into the patient’s ventilation, perfusion, and metabolism. During CPR, it is particularly useful because it acts as an indirect indicator of cardiac output and blood flow.
The main determinant of EtCO2 during CPR is effective chest compressions, which ensure that enough blood reaches the lungs to offload CO2. When compressions are performed properly, they enhance perfusion. This transports CO2 to the lungs, where it is then exhaled.
The Science Behind the Technique
Carbon dioxide is a waste gas, so why should you care about it? However, the reality is far from it. The blood level of carbon dioxide is as critically important as the blood oxygen levels. In fact, the amount of oxygen loaded into the hemoglobin that is transported to the tissues is highly dependent on the regulation of CO2. Moreover, carbon dioxide serves as the molecular signal, regulating both nervous and smooth muscle tissues.
In normal healthy individuals, EtCO2 levels closely correlate with arterial partial pressure of carbon dioxide (PaCO2). In the event of cardiac arrest, there will be a disruption in the blood flow and gas exchange. Nonetheless, EtCO2 will provide a noninvasive window into the quality of CPR chest compression to support better circulation and oxygen delivery to tissues.
How to Measure EtCO2?
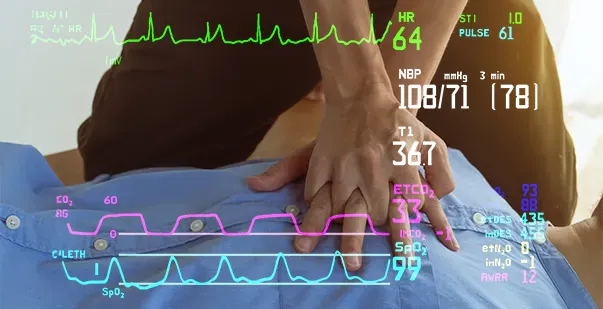
End Tidal CO2 mentoring is usually represented as a number and graph on a digital monitor. The number, known as capnometry, refers to the partial pressure of CO2 detected at the end of exhalation, ranging between 35-45 mm Hg. The waveform is known as a capnograph, which shows how much CO2 is presented at each phase of the patient’s respiratory cycle. It provides an integrated view of ventilation, perfusion, and metabolism. You can continuously monitor the EtCO2 levels through intubation and ventilation devices equipped with sensors.
Read more: What is Quantitative Waveform Capnography?
Where is EtCO2 Monitoring Used?
Before you find out what is the main determinant of end-tidal carbon dioxide, you should know where it holds a significant role. Exhaled CO2 monitors have been implemented as a standard of care in operating rooms for years. For instance, using CO2 monitoring in combination with pulse oximetry could prevent over 93% of anesthesia errors.
In recent days, it has been used much more in emergency settings, inside and outside the hospital. Some areas which are beginning to use end-tidal CO2 monitoring include,
- Ambulance services
- Emergency departments
- Procedural Care Units
- Post-Operative Units
- Intensive Care Units
These areas use capnography for various reasons, and each of them has witnessed improvement in patient outcomes.
What is the Main Determinant of End-tidal CO2 measurement During CPR?
The main determinant of EtCO2 during CPR is the quality and effectiveness of chest compressions. Proper chest compression, in this case, means the application of techniques that will pump oxygenated content blood from the heart into the lungs of the victim. This allows carbon dioxide in the bloodstream to be exchanged for air within the lungs. Therefore, enhanced chest compressions will enhance blood circulation around the body, including the lungs as a result of better perfusion of the lungs, enhanced clearance of carbon dioxide from the blood into the exhaled breath will occur.
Now that you know the answer, what is the main determinant of end-tidal carbon dioxide measurement during CPR? Let us know some key factors that influence the determinants of the EtCO2 monitoring. It includes,
-
Chest Compression Rate
Chest compression rate in CPR should be performed at 100-120 compressions per minute. Administer slower or faster than the specified administration rate might reduce the effectiveness and the outcomes of your resuscitation efforts.
-
Chest Compression Depth
When you are performing CPR, the chest compressions should depress the victim’s sternum at least 2 inches while not exceeding 2.4 inches in the case of an adult. If you perform the life-saving technique with insufficient depth, it might fail to facilitate the heart to pump adequate blood throughout the body.
-
Full Chest Recoil
After performing each chest compression in CPR, you must wait for a few seconds to allow the chest wall to return to its normal position. Maintaining the interval to allow full chest recoil will maximize the blood flow into the victim’s heart.
-
Minimum Interruptions
As chest compressions are the main determinant of end-tidal carbon dioxide, they should be administered continuously to the victims with no break or pause in between. You can take a pursuit to provide breaths or switch rescuers in emergency scenarios. Interrupts in between the chest compression will reduce the blood flow to the victim’s heart, thereby affecting the overall impact of CPR.
-
Chest Compression Fraction
While performing CPR on the victim, you should achieve a chest compression fraction rate of at least 60%. This means administering chest compressions should take up 60% or more of your total time providing cardiopulmonary resuscitation efforts.
Also read: What Is the Effect of Excessive Ventilation?
The Relationship Between EtCO2 and CPR
End-tidal CO2 monitor gives you an enormous amount of information during CPR, including the estimation of cardiac output, assessing the quality of chest compressions, and indicating when the patient has ROSC (Return of Spontaneous Circulation). Let us have a brief overview of each principle of EtCO2 in CPR.
-
Monitor Chest Compression Quality
Research after research emphasizes the importance of high-quality CPR, which can be challenging and elusive even for experienced professionals. Performing CPR is both physically and mentally demanding, as you have to repeat and administer compressions at the optimal depth and rate throughout the code.
EtCO2 monitoring will establish a baseline for assessing compression quality. If the reading is low, compressions are suboptimal and need improvement through retraining or ensuring full chest recoil. When you notice a gradual rise in the reading, it indicates improved perfusion from delivering stronger compressions.
-
Identify ROSC
A sharp, sudden increase in EtCO2 (>10 mmHg) is unlikely due to CPR alone and can be a reliable sign of ROSC. EtCO2 monitoring gives you an early, non-invasive sign of poor circulation return even before you can assess the victim’s heart rhythms. In such cases, you should check the patient thoroughly for spontaneous heartbeat or pulses. Additionally, it will also aid in minimizing the delays and interruptions in administering CPR.
-
Prognostic Information
Low and undifferentiated EtCO2 readings, deposing the ongoing chest compressions, indicate a poor prognosis. However, if the readings increase by 10 mmHg after 20 minutes of resuscitation efforts, then you can consider them as positive prognostic signs.
Moreover, the readings will help you make adjustments like switching compressors, providing ventilation, or prescribing drugs. The situation can be evaluated by monitoring EtCO2 response, where the rise provides reassurance that it is having a positive influence on your CPR efforts. Nonetheless, make sure to continue with CPR according to the guidelines.
Be the Best in Cardiac Care!
EtCO2 monitoring during CPR is a simple, non-invasive technique that enhances patient safety. Despite these benefits, it remains underutilized in cases of in-hospital cardiac arrest. This method is practical enough for routine use, provided healthcare professionals fully understand its principles and the main determinant of EtCO2 during CPR. The key factor is the effectiveness of chest compressions, which can be gauged through EtCO2 readings. High-quality compressions with the correct rate, depth, and recoil are linked to better patient outcomes during CPR. Thus, mastering this technique can optimize patient care in critical scenarios.
References
- What is the Main Determinant of EtCO2 During CPR?
- resuscitation-science-ETCO2.pdf
- Capnography during cardiac arrest – ScienceDirect
- The dynamic pattern of end-tidal carbon dioxide during cardiopulmonary resuscitation: difference between asphyxial cardiac arrest and ventricular fibrillation/pulseless ventricular tachycardia cardiac arrest – PMC
- Capnography during cardiac arrest
- End-tidal CO2 Detection of an Audible Heart Rate During Neonatal Cardiopulmonary Resuscitation Following Asystole in Asphyxiated Piglets – PMC