Table of Contents:
- Introduction
- Structure of the LAD Artery: Its Path and Branches
- Physiological Variants and Anomalies in LAD Anatomy
- What is LAD Stenosis? Causes and Severity Levels
- Symptoms of LAD Artery Blockage
- Clinical Significance of LAD Occlusion
- Diagnosing LAD Blockages: Tests and Imaging
- Treatment Options for LAD Stenosis and Blockages
- Prevent LAD Stenosis With The Right Strategy!
Introduction
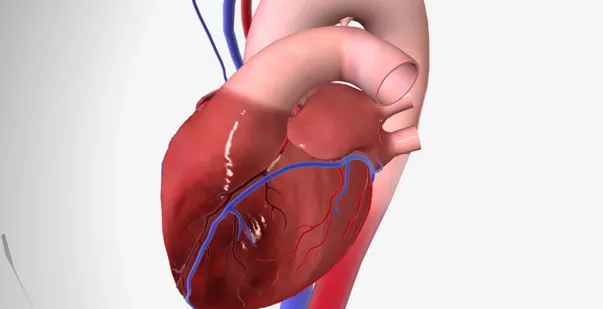
The Left Anterior Descending (LAD) artery, also known as the anterior interventricular artery (AIV), is one of the heart’s major blood vessels. As a branch of the left coronary artery, the LAD runs down the front of the heart. This artery supplies 50% of blood to the front part of the left ventricle and most of the interventricular septum. These areas are important for the heart’s pumping ability, which is why blockages in the LAD artery can be life-threatening. This artery is also often called the “widowmaker,” because a blockage here can stop blood flow to a large portion of the heart and cause severe heart attacks if not treated quickly.
In this post, we’ll explore the LAD artery’s structure, common problems like LAD stenosis and blockages, and how doctors diagnose and treat these conditions.
Master ACLS Now
Get ACLS certified with confidence
Structure of the LAD Artery: Its Path and Branches
The LAD artery begins at the left coronary artery. This artery follows the groove that separates the two ventricles on the front of the heart and curves around the bottom toward the back. It ends partway along the heart’s back surface, where it meets another artery, the right coronary artery. As the LAD travels along the heart, it gives off several smaller branches that supply key areas with oxygen-rich blood. The main branches of the LAD artery are:
- Conal Branch: This small branch supplies blood to a part of the right side of the heart’s front.
- Anterior Ventricular Branches: These branches go to both the right and left ventricles, with the left branches being larger and reaching more of the heart’s front surface.
- Interventricular Septal Branches: These branches supply blood to the interventricular septum, the wall separating the left and right ventricles. They specifically provide blood to the front two-thirds of this wall, which is required for carrying the electrical signals that control the heartbeat.
Physiological Variants and Anomalies in LAD Anatomy
In some people, the LAD may follow a unique course or have unusual structures. These variations can affect blood flow and heart health. They also become a deciding factor in surgical approaches to treating LAD-related issues.
-
Myocardial Bridging
Myocardial bridging occurs when a segment of the LAD artery runs intramurally beneath a bridge of myocardial tissue, typically over its mid-section. While often asymptomatic, this anatomical variant can lead to ischemia due to intermittent compression of the artery during systole.
-
Absent Left Main Artery
In rare cases, the left main coronary artery may be absent, resulting in the LAD and circumflex arteries originating separately from the aorta. This anatomical variation is critical to recognize during angiography and surgical planning. This can complicate stenting procedures and affect overall coronary circulation.
-
Coronary Artery Fistulae
Coronary artery fistulae represent abnormal connections between a coronary artery, such as the LAD, and a heart chamber or vein. Depending on their size and hemodynamic impact, these fistulae can disrupt normal blood flow dynamics.
Master ACLS Now
Get ACLS certified with confidence
What is LAD Stenosis? Causes and Severity Levels
LAD stenosis meaning that your LAD artery narrows, usually because of plaque buildup inside the artery walls. Plaque is made up of fat, cholesterol, and other substances that can stick to artery walls. Over time, plaque hardens and restricts blood flow.
Types of LAD Stenosis
LAD stenosis is measured by how much the artery has narrowed. This is typically classified as mild, moderate, or severe based on the LAD stenosis percentage as follows:
- Mild Stenosis (20-49% blocked): Blood flow is slightly restricted, often with no symptoms.
- Moderate Stenosis (50-69% blocked): Blood flow is more restricted and may cause symptoms, especially during exercise.
- Severe Stenosis (70-99% blocked): Blood flow is significantly restricted, causing symptoms even at rest, with a high risk of a heart attack.
Mild Mid LAD Disease
In mild mid LAD disease, the middle part of the LAD artery has some narrowing. This form of disease is only noticed during routine checkups, as it may not show symptoms right away. Mild cases may not need aggressive treatment but require lifestyle changes to prevent progression.
Also Read: Supraventricular Tachycardia: Causes, Symptoms, and Treatment Options
Symptoms of LAD Artery Blockage
A blockage in the Left Anterior Descending (LAD) artery can greatly reduce blood flow to the heart, especially when the heart needs more oxygen during physical activity or stress. LAD artery blockage symptoms vary among individuals but often include the following:
-
Angina Pectoris
Angina, a pressing or squeezing chest pain, occurs when blood flow through the LAD artery is restricted, especially during activity or stress. This pain may radiate to the left arm, jaw, back, or shoulders, signaling reduced oxygen supply to the heart muscle.
-
Shortness of Breath
Reduced blood flow in the LAD can lead to dyspnea, or shortness of breath, even during minimal exertion. The heart struggles to pump effectively, causing fluid buildup in the lungs and resulting in breathlessness, especially in severe cases.
-
Palpitations and Fatigue
With poor blood supply to the heart, patients may feel palpitations (an abnormal heartbeat sensation) and chronic fatigue. This happens because the heart works harder to pump blood, reducing its efficiency and leading to an overall energy drain.
-
Dizziness or Lightheadedness
Due to insufficient oxygenated blood reaching the brain, dizziness or lightheadedness may occur, particularly during exertion or sudden changes in position. This can increase the risk of falls and may signal severe heart compromise.
-
Sweating (Diaphoresis)
Cold sweats or excessive sweating, often unexplained, can be a sign of heart strain. This symptom is common during angina episodes and indicates the body’s stress response to a lack of adequate blood flow through the LAD.
-
Nausea and Vomiting
Nausea, sometimes accompanied by vomiting, may occur due to the body’s reaction to reduced blood flow in the heart muscle, especially in severe LAD blockages. This symptom often accompanies other cardiac distress signs, like chest pain and sweating.
Clinical Significance of LAD Occlusion
A blockage in the LAD artery can be life-threatening as it supplies blood to essential parts of the heart. When LAD blood flow is reduced, the heart’s front wall suffers. This condition is identified by specific ECG changes, like ST-segment elevation in leads V1-V4, which indicate a high-risk heart attack area.
-
Wellen’s Syndrome and Early Detection
Wellen’s syndrome is an early sign of LAD blockage. It is detected through distinctive T-wave patterns in an ECG. This pattern signals a high risk for a future heart attack. Thus, patients should receive immediate treatment.
-
LAD 90 Blockage and Widowmaker Artery
A 90% blockage in the LAD presents an urgent risk for complete occlusion. Known as the “widowmaker,” this artery’s blockage often leads to fatal myocardial infarctions, particularly affecting the left ventricular anterior wall.
Diagnosing LAD Blockages: Tests and Imaging
Doctors use different tests to find LAD stenosis and other coronary artery problems. These tests help determine the blockage level and the best treatment plan. Following are the tests that doctors may order to confirm LAD stenosis:
-
Coronary Angiography
Coronary angiography is a diagnostic procedure that uses X-ray imaging to visualize the coronary arteries, which supply blood to the heart. In this procedure, a special dye is injected into the arteries through a catheter. This helps detect narrowing or blockages in the arteries.
-
Electrocardiogram (ECG)
An ECG records the heart’s electrical signals to detect abnormalities caused by blockages in the LAD artery. The test looks for specific patterns, like changes in the ST segment or T-waves, which can indicate blood flow issues in the heart muscle.
-
Stress Testing
During a stress test, doctors evaluate how the heart performs under physical stress or medication-induced strain. The test monitors blood flow and heart rate to detect blockages like those in the LAD. Restricted blood flow during stress may point to a narrowing in the artery. This helps doctors assess blockage severity and plan further tests.
Also Read: What is the difference between cardiac arrest and a heart attack?
Treatment Options for LAD Stenosis and Blockages
Treatment options for LAD artery blockages depend on the severity of the narrowing and the patient’s overall health. They can range from lifestyle changes and medications to invasive procedures.
-
Medical Treatment and Lifestyle Changes
For mild to moderate LAD stenosis, medications and lifestyle adjustments are often effective in managing symptoms and slowing disease progression. Beta-blockers, ACE inhibitors, and nitrates can reduce chest pain and improve blood flow. Patients should also adopt certain lifestyle changes, such as quitting smoking, eating a healthy diet, and exercising regularly. They are important to reduce risk factors and prevent further narrowing of the LAD artery.
-
Stenting in LAD Blockages
Stenting is a procedure often used for severe blockages in the LAD. During percutaneous coronary intervention (PCI), doctors insert a thin tube, or stent, into the narrowed artery section to keep it open. This stent restores normal blood flow and reduces symptoms like chest pain and shortness of breath. Inserting a stent in LAD is a minimally invasive option that often provides long-lasting relief from symptoms.
-
Coronary Artery Bypass Grafting (CABG)
In cases of multiple or severe blockages, CABG surgery may be required. In this procedure, surgeons use a healthy blood vessel from another body part to bypass the blocked LAD artery. This alternative path for blood flow ensures the heart muscle gets enough oxygen and reduces the risk of a heart attack. CABG is more invasive than stenting but can be highly effective for complex blockages, especially when combined with lifestyle changes.
Prevent LAD Stenosis With The Right Strategy!
The Left Anterior Descending (LAD) artery supplies blood to large sections of the heart muscle. Any blockage or stenosis in this artery can lead to serious conditions, including heart attacks and heart failure. To prevent LAD disease progression, patients are advised to prioritize lifestyle changes such as managing stress and regular health checkups. Staying aware of cholesterol and blood pressure levels can also reduce risks of atherosclerosis in the LAD.
For those interested in advanced heart health skills, Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS) training offer practical knowledge for managing cardiac emergencies, such as heart attacks related to LAD blockages.
References: