Table of Contents:
- What is Transcutaneous Pacing (TCP)?
- When is Transcutaneous Pacing used in ACLS?
- Preparing for Transcutaneous Pacing
- Step-by-step guide to Transcutaneous Pacing
- Troubleshooting common TCP Issues
- Conclusion
Advanced Cardiovascular Life Support (ACLS) is a crucial procedure for handling cardiac crises in the high-stakes field of emergency care. Transcutaneous pacing is a must-have tool among its array of life-saving strategies for treating severe bradycardia and heart blockages.
Transcutaneous pacing is an important, non-invasive strategy in ACLS that may stabilize patients with severe bradycardia or heart blockages. Acting quickly will help it to be very successful. Studies using transcutaneous pacing either prophylactically or within five minutes of asystolic cardiac arrest suggest success rates perhaps exceeding 90%. This approach can save lives in catastrophic cardiac crises. Our detailed guide demystifies transcutaneous pacing ACLS and equips healthcare professionals to handle these difficult situations.
We will take you through every important stage, from equipment setup to troubleshooting.
Master ACLS Now
Get ACLS certified with confidence
What is Transcutaneous Pacing (TCP)?
Transcutaneous pacing (TCP) is a short, non-invasive technique of cardiac pacing used in emergencies to treat severe bradycardia or heart blockages. It stimulates the heart muscle by passing electrical impulses via electrodes put on the patient’s skin, therefore regulating the heart rate. Setting the pacing device to a specified demand rate for transcutaneous pacer guarantees it only generates impulses when the heart’s natural rate drops below this level.
There are several types of TCP electrodes, each intended for specific clinical scenarios:
- One Step Pacing Electrodes streamline the procedure by integrating ECG monitoring capabilities.
- One-Step Complete Electrodes include defibrillation, monitoring, and pacing capabilities.
- Standard Anterior-Posterior Electrodes are set up traditionally with one electrode on the chest and another on the back.
- Transvenous Electrodes, although not exactly transcutaneous, are inserted into the heart for more direct pacing.
- Epicardial Electrodes have been implanted directly on the heart’s surface.
The therapy environment, available tools, and the patient’s particular requirements determine the kind of electrode to be used. Proper electrode placement is crucial for effective pacing and pain reduction.
Medical teams may advise the anterior-posterior posture in crises. This placement involves putting one electrode on the chest and another on the back. Such posture enables the efficient delivery of electrical impulses to the heart. Healthcare professionals should become familiar with different electrode types and installation methods. This information helps them to provide the finest treatment available and react fast to various situations.
When is Transcutaneous Pacing Used in ACLS?
Transcutaneous pacing in ACLS is predominantly employed in cases of symptomatic bradycardia, particularly when indicators of inadequate perfusion are evident. Here are the key points regarding the use of TCP in ACLS:
-
Indication
Patients with symptomatic bradycardia showing evidence of inadequate perfusion should use TCP. This includes symptoms like changed mental state, hypotension, or shock signals. TCP’s ability to provide required cardiac stimulation helps to save lives in these dire circumstances.
-
Preparation
Atropine may be administered while preparing to initiate transcutaneous pacing to attempt to alleviate bradycardia. TCP should be started right away; however, should atropine prove insufficient or the patient’s condition be severe, quick action is required to maintain suitable circulation.
-
Timing
TCP should not be delayed in individuals with symptomatic poor perfusion. The main question asked is, ‘what is your initial impulse setting for a transcutaneous pacemaker?‘. The answer typically involves setting a relatively high output, often around 60 and 90 beats per minute, to ensure effective myocardial capture. The initial pace rate changes depending on the patient’s clinical reaction. Effective pacing depends on ongoing observation and evaluation.
-
Contraindications
TCP is contraindicated in hypothermia patients as bradycardia might be a normal reaction to lower metabolic rates in such situations. TCP is not advised for people with asystole, either. Other ACLS procedures should be used in these situations.
-
Assessment
Since TCP might produce muscle movements that could resemble a pulse, it is advisable to evaluate circulation during the surgery using the femoral pulse instead of the carotid pulse. This ensures an accurate evaluation of the patient’s hemodynamic response to pacing.
Read More: How Many Ceus For ACLS
Master ACLS Now
Get ACLS certified with confidence
Preparing for Transcutaneous Pacing
Effective transcutaneous pacing steps in ACLS depend on correct preparation. Let us look at the points that one needs to keep in consideration at all times:
-
Necessary Equipment
Before beginning transcutaneous pacing ACLS, get all the necessary equipment. You’ll want conductive gel, a defibrillator/pacer device, ECG electrodes, and pacing pads. Also, make sure you have a functioning suction device and airway management equipment available.
Check that the defibrillator/pacer unit is fully charged and functioning properly. It is always a good idea to have additional pace pads available in case the first set encounters problems.
-
Patient Preparation
Effective pace depends on good patient preparation. If the patient is aware, start by walking them through the process. Clean and dry the area of skin where you plan to place the pads. If necessary, shaving any chest hair guarantees good contact.
Position the pads correctly – usually one on the front left chest and one on the back. If back access is limited, place the second pad on the left side under the armpit. Apply conductive gel to the pads for enhanced electrical transmission.
-
Safety Precautions and Considerations
Safety is the most important aspect of transcutaneous pacing ACLS. Remove any metal jewelry and medical patches from the patient’s chest region. Keep oxygen sources away from the pacing site to reduce the danger of fire. Ensure that all team members understand their tasks and remain clear of the patient during shock delivery.
The patient’s vital signs should be monitored continually during the treatment. Also, be prepared to deal with possible problems such as skin burns or patient discomfort. Pacing may generate muscular twitching that may resemble a pulse; therefore, always check for actual cardiac capture.
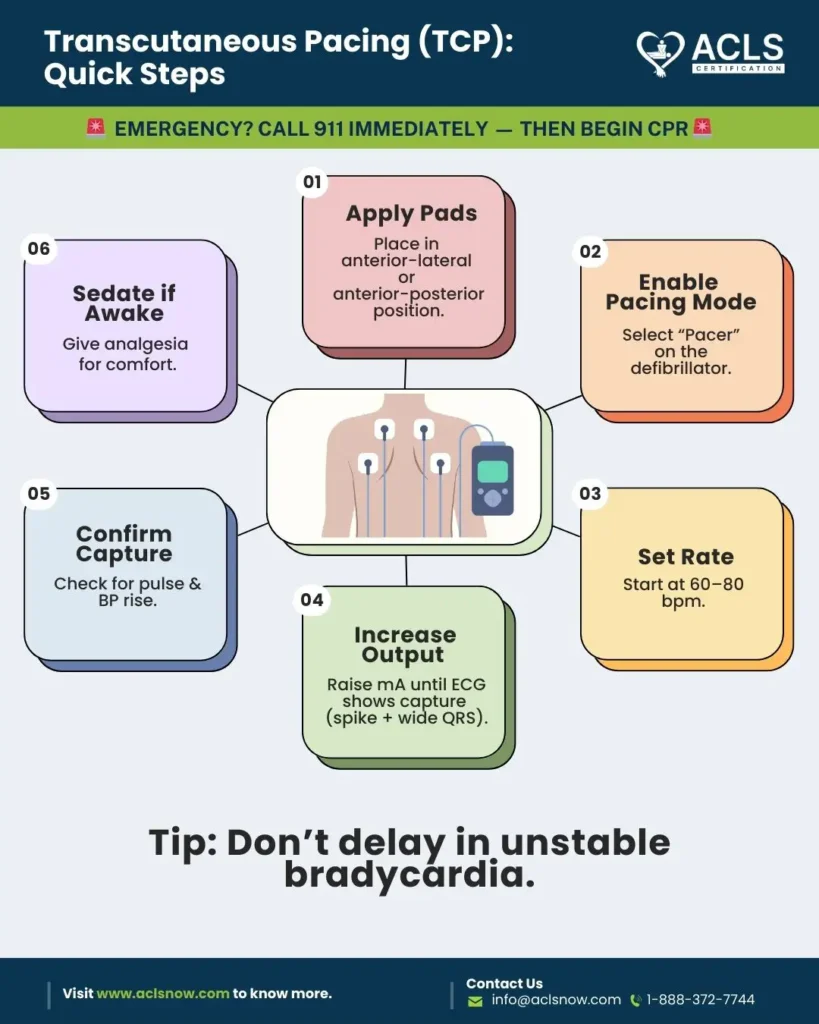
Step-by-Step Guide to Transcutaneous Pacing
The transcutaneous pacing step is a critical skill in ACLS that can save lives during severe bradycardia or heart blocks. Let’s walk you through the safe and successful transcutaneous pacing technique. Following these steps will help you be ready to handle this essential intervention in an emergency.
-
Preparation
Before beginning transcutaneous pacing steps in ACLS, collect all essential equipment, including the transcutaneous pacer, electrodes, conductive gel, and ECG monitoring devices. Effective pace and patient safety depend critically on good hand hygiene and sterile technique.
To execute the process quickly, make sure your workstation is neat and orderly. Spend some time familiarizing yourself with the particular pacer model you will be using, as various devices may have somewhat different interfaces or features.
-
Electrode Placement
Correct electrode placement is essential for effective transcutaneous pacing in ACLS. There are two main options to consider:
- Anterior-Posterior: Put one electrode on the chest, slightly left of the sternum. Lay the second electrode straight behind the heart on the back. Usually, this arrangement offers the best stimulation of the cardiac muscle.
- Anterior-Lateral: Place one electrode on the left side of the chest, near the apex of the heart. Then, lay the second electrode on the lateral chest wall under the left armpit. This arrangement may help when access to the patient’s back is restricted.
Apply a lot of conductive gel for both choices to increase electrical contact. Make sure the electrodes are securely fixed to the skin to guarantee a constant pace throughout the operation.
-
Initiating TCP
When thinking about what steps should be followed to start pacing, begin by connecting the electrodes to the pacer device. Turn on the machine and then choose the suitable pace setting. Based on the patient’s state, set the first pace rate—usually between 60 and 90 beats per minute. Start with modest milliamps (mA), usually between 20 and 30 mA. Mind patient comfort and the danger of skin burns at increasing energy levels as you progressively up the mA until capture is achieved.
-
Verifying Capture
Transcutaneous pacing stages mostly consist of confirming capture. Look for:
- Electrical Capture: Wide QRS complex on ECG after each pacing spike.
- Mechanical Capture: This occurs when you can feel a pulse that matches the set pacing rate, confirming that the electrical impulses are effectively causing the heart to contract and pump blood.
If capture is not received, try adjusting electrode location or increasing mA. Complete capture on an ECG will reveal consistent, broad QRS complexes after every pacing pulse.
-
Monitoring and Adjustments
Continuous monitoring is important. Keep a close eye on:
- ECG rhythm
- Blood pressure
- Oxygen saturation, in general
- Patients’ comfort and responsiveness
Adjust pacing parameters as needed. If capture is lost, you may need to raise the mA. If the patient is uncomfortable, decrease the mA. The goal is to capture reliably at the lowest feasible mA.
Read More: What To Do When Your ACLS Has Expired
Master ACLS Now
Get ACLS certified with confidence
Troubleshooting Common TCP Issues
Sometimes, ACLS transcutaneous pacing is difficult. This is how to approach typical problems:
-
Failure to Capture
Problem: The pacemaker is not sufficiently stimulating the heart.
Solution:
-
- Check the electrode location to ensure it is in inappropriate contact with the skin.
- Change the output parameters; increase the current until capture is reached.
- Ensure the skin is free from too much dampness or hair that can hinder conduction.
-
Inadequate Pacing Rate
Problem: Bradycardia results from a pacing rate that is too low.
Solution:
-
- Raise the pace to the recommended range—typically 60–90 beats per minute.
- Track the patient’s reaction and make required corrections.
-
Skin Burns or Irritation
Problem: Prolonged contact with electrodes can cause skin irritation or burns.
Solution:
-
- Look at the skin beneath the electrodes regularly.
- Adjust electrode location if irritation develops.
- Use conductive gel or pads meant to cause the least possible skin injury.
-
Loss of Pacing
Problem: The pacing stops unexpectedly.
Solution:
-
- View the pacing device’s battery level.
- Check the wires and connectors for faults or disconnections.
- Make sure the pacing mode is in the proper setting.
-
Patient Discomfort
Problem: The patient finds pace to be uncomfortable or painful.
Solution:
-
- Change the pace output so that it maintains capture but lessens pain.
- If the patient is uncomfortable or worried, think about sedation.
-
Interference from External Devices
Problem: Pacing may be interfered with by other electronics.
Solution:
- Move the patient away from powerful electrical fields and MRI equipment, among sources of electromagnetic interference.
- Verify equipment’s appropriate grounding.
Final Thoughts
Transcutaneous pacing in ACLS is an essential skill for healthcare providers managing severe bradycardia and heart blocks. When used right away and properly, this noninvasive approach may be literally life-saving. TCP is just a temporary fix for patients before definitive therapy can start. You should always be learning and improving your knowledge and skills through consistent training and practice.
Stay prepared, as your TCP knowledge might make the difference in a cardiac emergency. Consult the most recent ACLS recommendations and look for opportunities for practical training for more specific procedures.