Table of Content(s)
- Introduction
- What are the symptoms of PEA and Asystole?
- What are the causes of asystole?
- What are the causes of PEA?
- PEA vs Asystole: Know the difference
- What is the ideal recommendation of Vasopressors for Asystole?
- What is the ideal recommendation of Vasopressors for PEA?
- Conclusion
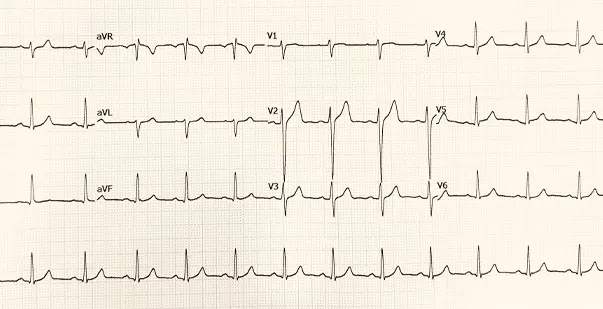
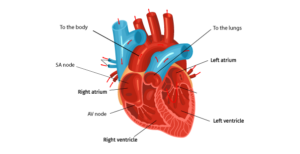
PEA or Pulseless Electrical Activity is a clinical condition where the heart’s muscles fail to respond to the heart’s electrical activity. This results in ineffective contractions and the inability to produce a pulse.
Asystole on the other hand is a state of cardiac arrest. In this condition the heart fails to generate any electrical activity. Asystole is detected as a flatline in an ECG (electrocardiogram).
The first thing to mention in the topic of Asystole vs PEA is that both of these conditions are potentially fatal, if left undiagnosed. Therefore, swift and rapid detection is the key to saving lives. Even though both PEA and Asystole are types of cardiac arrest, they differ significantly in underlying mechanisms. The causes, treatment and even the approach differs for the two. This blog aims to help you understand the differences between these two conditions. By properly distinguishing, you will be able to respond effectively in these high stake situations.
What are the symptoms of PEA and Asystole?
Both Pulseless Electrical Activity (PEA) and Asystole represent severe forms of cardiac arrest. But they have distinct clinical presentations. Recognizing the symptoms and understanding the differences is crucial for timely and effective intervention.
Symptoms of Pulseless Electrical Activity (PEA):
- Absence of Pulse: Despite organized electrical activity on the ECG, there is no palpable pulse or measurable blood pressure.
- Loss of Consciousness: The patient is unconscious and unresponsive due to lack of adequate blood flow to the brain.
- Respiratory Arrest: The patient is not breathing or shows inadequate breathing.
- Pale or Cyanotic Skin: The skin may appear pale or bluish due to poor oxygenation.
- Cold Extremities: The extremities may feel cold to the touch, reflecting poor circulation.
Symptoms of Asystole:
- Flatline ECG: Complete absence of electrical activity on the ECG, presenting as a flatline.
- No Pulse: There is no detectable pulse or blood pressure.
- Loss of Consciousness: The patient is unconscious and unresponsive due to a lack of effective cardiac output.
- Respiratory Arrest: The patient is not breathing or exhibits inadequate breathing.
- Pale or Cyanotic Skin: The skin may appear pale or bluish, indicating severe lack of oxygenated blood.
What are the causes of Asystole?
Asystole is a severe form of cardiac arrest. It is marked by the absence of electrical or mechanical heart activity. Asystole demands immediate intervention, otherwise it can be fatal. These are the common causes of asystole:
- Hypoxia: Insufficient oxygen supply to the body’s tissues, particularly the heart.
- Hypovolemia: Severe blood or fluid loss, leading to inadequate blood circulation.
- Hyperkalemia: Elevated potassium levels in the blood, affecting heart function.
- Hypothermia: Critically low body temperature, slowing down all physiological processes.
- Tension Pneumothorax: Air accumulation in the pleural space, causing lung collapse and impaired heart function.
- Cardiac Tamponade: Fluid buildup in the pericardium, restricting heart movement.
- Toxins: Exposure to certain drugs or poisons that affect cardiac function.
- Massive Myocardial Infarction: Extensive heart muscle damage due to a heart attack.
- Acidosis: Severe blood pH imbalance, often metabolic or respiratory in origin.
- Pulmonary Embolism: Blockage in the pulmonary artery, impairing blood flow to the lungs and heart.
Read More: Things You Need to Know About PEA
What are the causes of Pulseless Electrical Activity (PEA)?
Pulseless Electrical Activity or PEA is a clinical condition where the heart fails to contract effectively. This happens due to no palpable pulse or blood circulation. Prompt identification of the underlying causes are essential for successful resuscitation. Here are the common causes of PEA:
- Massive Pulmonary Embolism: A large blood clot in the lungs, obstructing blood flow and leading to inadequate oxygenation.
- Severe Hypovolemia: Extreme blood or fluid loss causing insufficient circulating blood volume to maintain cardiac output.
- Acute Myocardial Infarction: Heart attack leading to significant damage to the heart muscle, impairing its ability to contract.
- Tension Pneumothorax: Air accumulation in the pleural space, causing lung collapse and increased pressure on the heart.
- Cardiac Tamponade: Fluid buildup in the pericardial sac. This compresses the heart and restricts its normal movement.
- Severe Acidosis: A critical imbalance in blood pH levels, affecting cardiac and cellular function.
- Severe Electrolyte Imbalances: Abnormal levels of electrolytes such as potassium, calcium, and magnesium, disrupting cardiac electrical activity.
PEA vs Asystole: Know The Difference
Distinguishing between Pulseless Electrical Activity (PEA) and Asystole is critical for timely management and treatment. Both conditions are present during cardiac arrest and require immediate action. They however differ in their underlying mechanisms, clinical presentation, and management strategies. Understanding these differences are important:
| Pulseless Electrical Activity | Asystole |
| Organized electrical activity is present on the electrocardiogram (ECG). There is no effective mechanical heart contraction, resulting in no palpable pulse. | There is a complete absence of electrical activity on the ECG. It is indicated by a flatline, and no mechanical heart activity or pulse. |
| Resembles normal sinus rhythm or other identifiable rhythms. | Displays a flatline on the ECG with no detectable electrical activity. |
| Caused by reversible conditions such as severe hypovolemia, hypoxia, tension pneumothorax, cardiac tamponade, massive pulmonary embolism, severe acidosis, and electrolyte imbalances. | Generally associated with severe, irreversible conditions such as extensive myocardial infarction, prolonged hypoxia, severe acidosis, and advanced cardiac disease. |
| Focuses on identifying and treating underlying reversible causes. | Immediate initiation of CPR and epinephrine administration, with a focus on identifying and treating any reversible causes. |
| Prognosis can vary widely depending on the rapidity and effectiveness of identifying and treating the underlying cause. | Prognosis is generally poor due to the lack of electrical and mechanical activity, making successful resuscitation less likely. |
What is the ideal recommendation of Vasopressors for Asystole?
The primary goal of managing asystole is to restore cardiac function. Along with that, the second most important goal is increasing the chances of successful resuscitation. Vasopressors enhance blood flow to vital organs and support the circulation during cardiac arrest. This is the ideal recommendation of vasopressors in asystole:
- Epinephrine: Administer 1 mg every 3-5 minutes during CPR (cardiopulmonary resuscitation). Epinephrine increases myocardial and cerebral perfusion pressure. This enhances the likelihood of ROSC (Return of Spontaneous Circulation).
- Vasopressin: Not used as a mandate, but often used as an alternative.
- Norepinephrine: Typically not used as a first-line agent in the management of asystole. Norepinephrine may be utilized in other critical scenarios, such as severe hypotension.
Check out the ACLS algorithm for Arrhythmias.
Read More: Is ACLS Medical Training Legit?
What is the ideal recommendation of Vasopressors for PEA?
In pulseless electrical activity, the role of vasopressors is to support circulation and restore pulse. These are the ideal recommendations of ACLS medications for PEA:
- Epinephrine: Administer at a dose of 1 mg every 3-5 minutes during cardiopulmonary resuscitation (CPR), same as the line of treatment for Asystole.
- Treatment for Reversible Causes: Identify and address any underlying reversible causes of PEA. This includes hypoxia, hypovolemia, cardiac tamponade, or tension pneumothorax. Treating these causes can significantly impact the success of resuscitation efforts.
Conclusion
Understanding the differences between Asystole vs PEA, is critical for anyone in the ACLS forefront. Both of these conditions are extremely serious and demand immediate action. They present unique challenges and must be handled with different, tailor-made approaches.
Apart from all the differences, both of these conditions highly rely on quality cardiopulmonary resuscitation (CPR). The line of treatment also includes timely use of vasopressors, comprehensive assessment followed by treatment. You can enroll in an Advanced Cardiovascular Life Support (ACLS) training class and master the differences between asystole and PEA. With the right training, you can be equally capable of delivering care with greater precision and effectiveness.