The PALS (Pediatric Advanced Life Support) cardiac arrest algorithm is a comprehensive set of guidelines aimed at aiding healthcare providers in managing cardiac arrest cases in pediatric patients. It offers a structured approach to resuscitation, ensuring that timely and effective interventions are administered to enhance patient outcomes. This algorithm outlines a series of sequential steps to be followed during a pediatric cardiac arrest, including assessing the patient's responsiveness, initiating CPR (Cardiopulmonary Resuscitation), administering medications, and providing advanced life support measures. By following this algorithm, healthcare providers can respond swiftly to pediatric medical emergencies, thereby improving the chances of a positive outcome. Early intervention is crucial in saving lives during cardiac arrest, and adhering to these sequential steps enables healthcare teams to provide prompt and efficient care to pediatric patients in distress.
Explanation of Flow Chart
- Scene Assessment:
- Check the scene for safety
- Shout for help and call emergency services.
- Start CPR if the child is not breathing/gasping, and/or doesn’t have pulse
- Initiate CPR: 15:2 ratio if no advanced airway
- Administer oxygen, ventilate with bag-mask
- Attach defibrillator (AED)
- Automated External Defibrillation: Check for a shockable rhythm
- If a shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) is detected
- Deliver a shock immediately.
- If no shockable rhythm is detected
- Administer epinephrine (0.01 mg/kg every 3-5 minutes, max dose 1mg)
- CPR with cycles (15:2 if no advanced airway) of compressions and ventilations.
- Continue CPR
- Provide 15 chest compressions followed by 2 ventilations.
- If an advanced airway is in place, deliver 1 breath every 2-3 seconds.
- Use medications( epinephrine (0.01 mg/kg, Amiodarone 5 mg/kg bolus, max dose: 3 doses, and Lidocaine 1 mg/kg loading dose).
- Repeat shock delivery with a defibrillator.
- If you receive a signal, deliver the shock.
- Check for recovery signs:
- If ROSC is achieved, monitor the child’s vital signs and continue supportive care.
- If no ROSC, continue CPR (step 5) and reevaluate rhythm and interventions.
Key components of the PALS cardiac arrest algorithm include:
- Early recognition and activation: Healthcare providers must promptly recognize cardiac arrest symptoms and activate the emergency response.
- Basic life support: This includes initiating high-quality CPR with chest compressions, delivering rescue breaths, and using an AED, if available.
- Advanced cardiovascular life support: Once advanced life support measures are initiated, healthcare providers focus on optimizing circulation and oxygenation through interventions such as intravenous administration of medications (e.g., epinephrine), and advanced airway management.
- Reversible causes: In medical emergencies, it is imperative to review the reversible causes; they can often stabilize the patient by intervening on the specific cause of cardiac arrest. The H’s and T’s are: Hypovolemia, Hypoxia, Hydrogen Ion (acidosis), Hypoglycemia, Hypo/Hyperkalemia, Hypothermia, Tension pneumothorax, Tamponade (cardiac), Toxins, and Thrombosis (pulmonary, cardiac)
- Post-resuscitation care: Once the patient stabilizes, the healthcare providers shift their focus to post-cardiac arrest care, including targeted temperature management, hemodynamic support, and treating the underlying cause of the arrest.
- Recovery Position: The recovery position helps you place an unconscious but breathing individual on their side. Their upper leg must stay bent and the head tilted back, to maintain an open airway and prevent aspiratio.
Sources
- American Heart Association. Pediatric Advanced Life Support Algorithms. Retrieved from https://osteopathicfounders.org/wp-content/uploads/2021/01/PALS-Algorithms-2020.pdf
- Performance of a consensus scoring algorithm for assessing pediatric advanced life support competency using a computer screen-based simulator. Pediatric Critical Care Medicine. Retrieved from https://journals.lww.com/pccmjournal/Fulltext/2009/11000/Performance_of_a_consensus_scoring_algorithm_for.1.aspx
- Duff JP, Topjian A, Berg MD, et al. The use of high-dose epinephrine for patients with out-of-hospital cardiopulmonary arrest is refractory to prehospital interventions. Pediatric Emergency Care. 2005;21(4):227-237. https://pubmed.ncbi.nlm.nih.gov/15824681/
- iming and Identification of the Cause and Treatment of a Cardiac Arrest: A Potential Survival Benefit Philippe Dewolf, a ,* Lina Wauters, a G https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9485947/#:~:text=The%20most%20frequent%20reversible%20causes,%2C%20and%20toxins%20%5B3%5D
- What is the best position to place and re-evaluate an unconscious but normally breathing victim? A randomised controlled human simulation trial on children https://www.sciencedirect.com/science/article/abs/pii/S0300957218310657
All PALS Algorithms
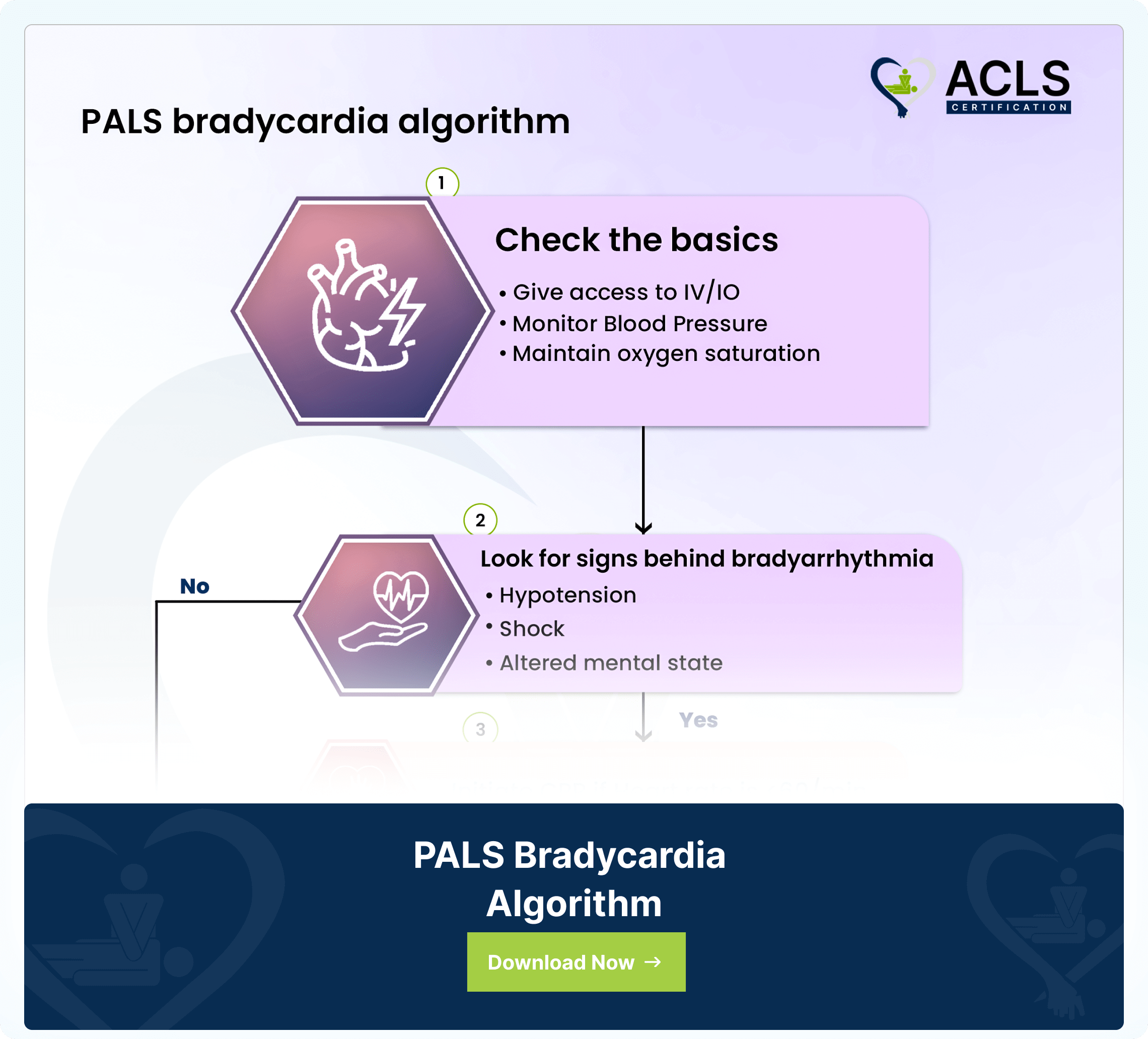
PALS Bradycardia Algorithm
The Pediatric Advanced Life Support (PALS) Bradycardia Algorithm gives a systematic approach to managing slow heart rates
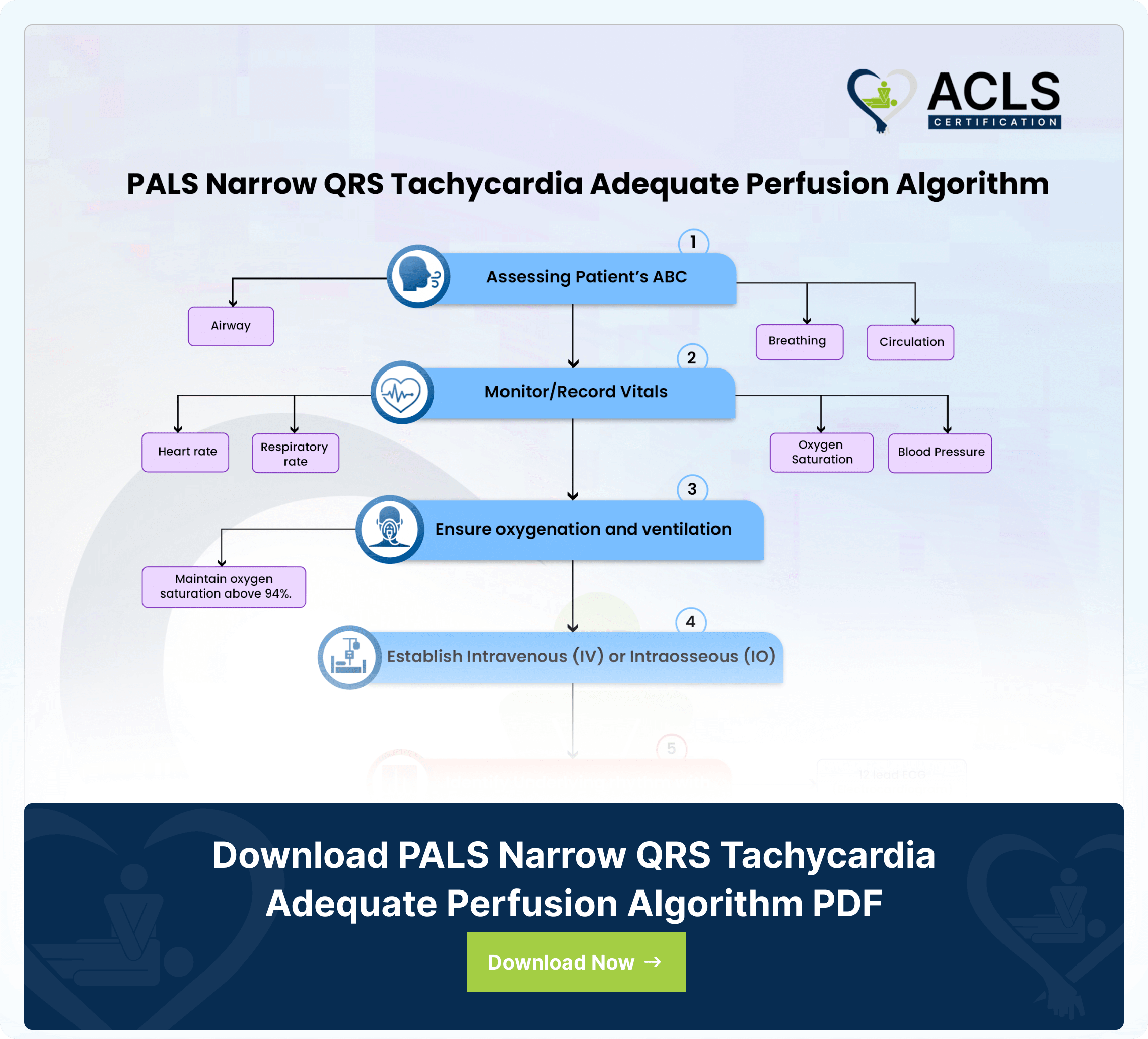
PALS Narrow QRS Tachycardia Adequate Perfusion Algorithm
The PALS Narrow QRS Tachycardia Adequate Perfusion Algorithm gives a structural approach for managing pediatric cardiac emergencies. The algorithm ensures effective treatment to maintain adequate perfusion in pediatric patients.
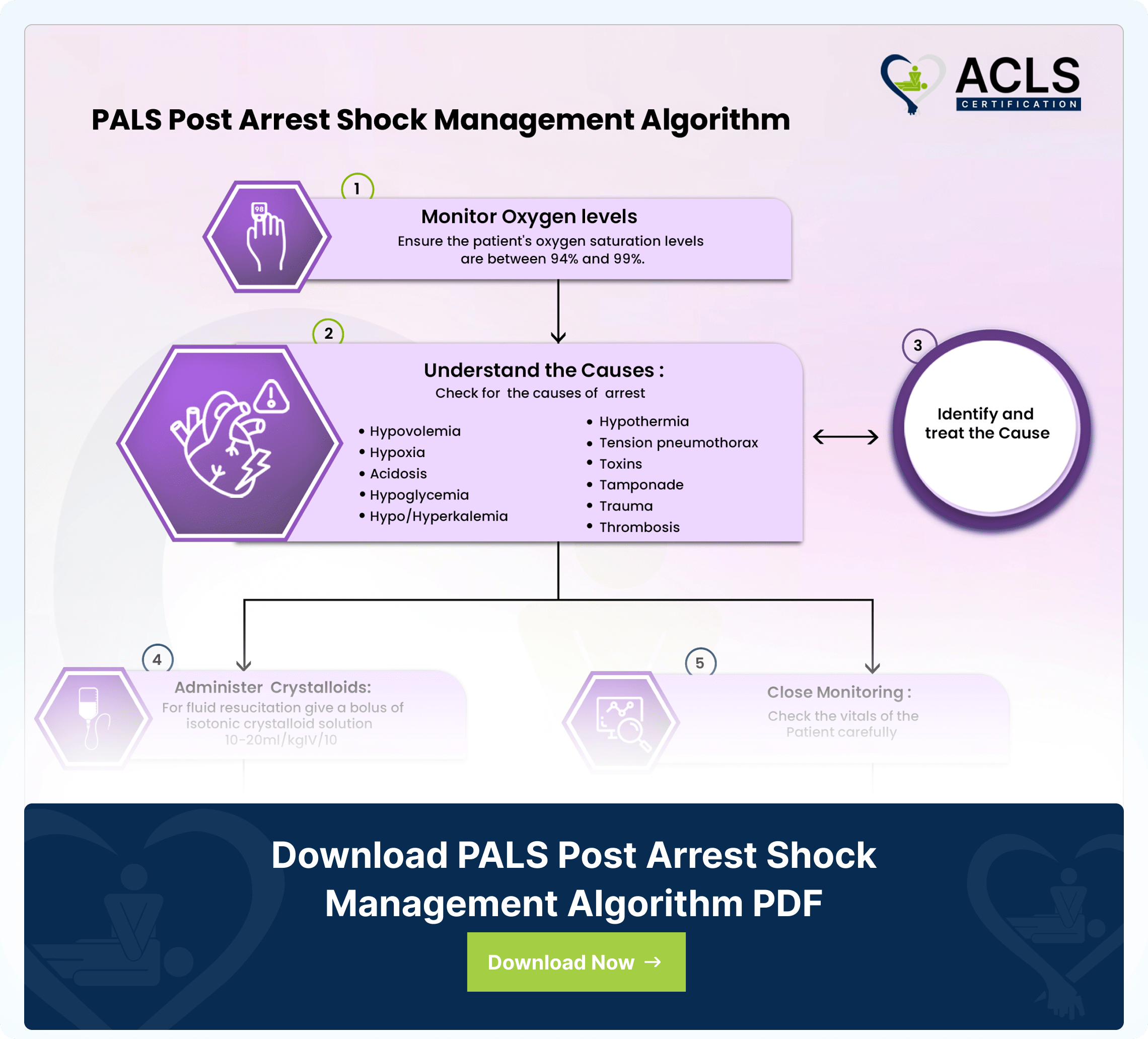
PALS Post Arrest Shock Management Algorithm
The PALS Algorithm Stabilizes pediatric patients’ post-cardiac arrest optimizing recovery through targeted interventions