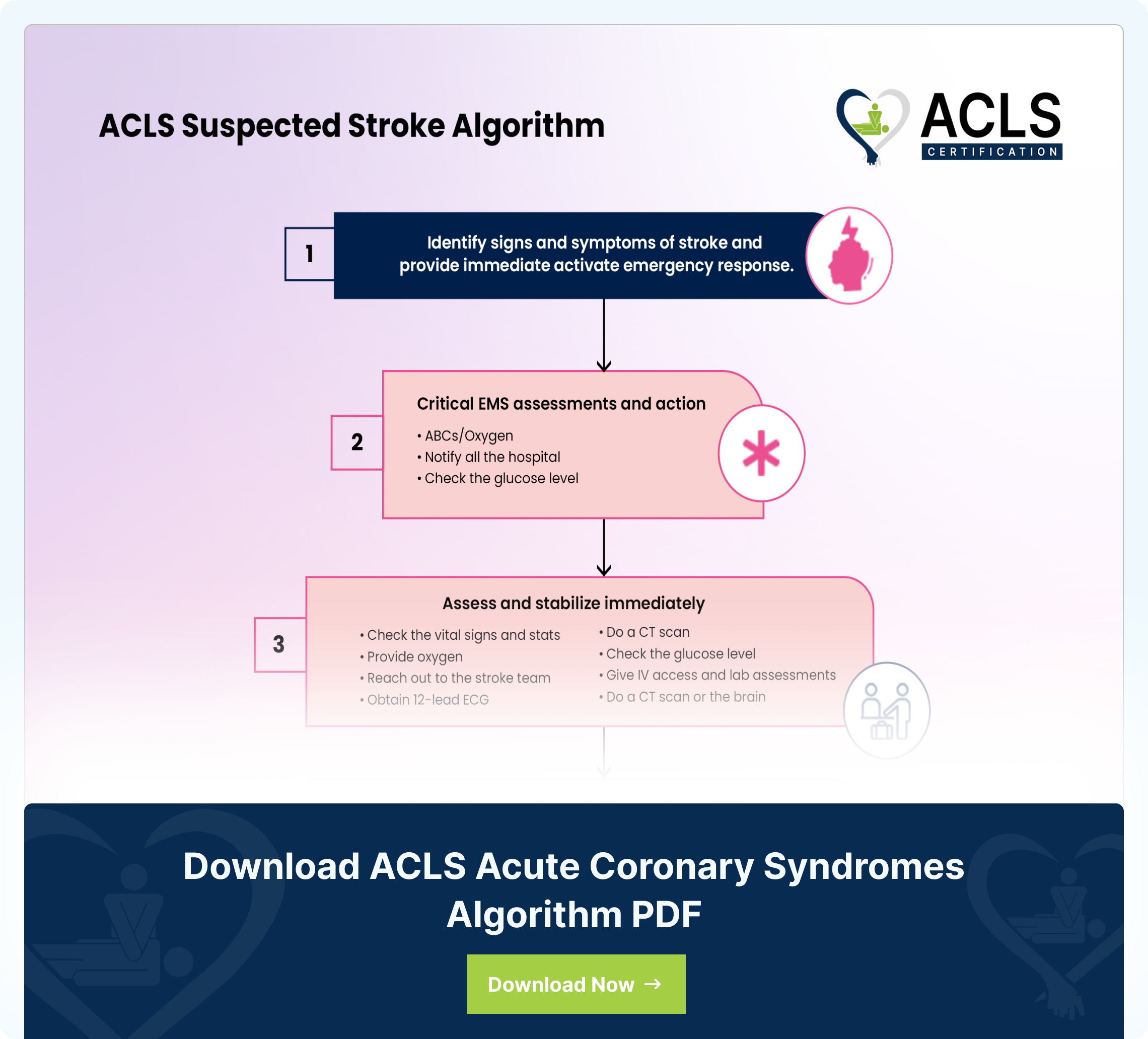
The ACLS Suspected Stroke Algorithm is a systematic approach, intended to manage patients suspected of having a stroke. It involves recognizing the symptoms using the FAST (face, arms, speech, and time) method and activating the emergency response system. The next step is providing supportive care and ensuring that the airway, breathing, and circulation are well-maintained, followed by rapid transportation. The key steps include assessing and maintaining the patient’s airway, and circulation followed by a neurological examination. The neurological examination assesses the nervous system, coordination, balance, sensory perception, motor dysfunction, and more. The providers implement targeted interventions such as conducting CT (Computed Tomography) scans, administration of fibrinolytic agents, assessment of ABCs, and readiness for transition to care for invasive interventions, if needed. The algorithm then directs providers to initiate the right interventions such as assessment of blood glucose. Below is the flowchart of an ACLS suspected stroke algorithm.
Step by step analysis of flowchart
- Identify signs and symptoms of a possible stroke and an active emergency response:
Observe the patient for signs of a stroke. Use F-A-S-T to remember symptoms such as unilateral facial drooping, arm weakness, speech difficulties, and call 9-1-1 in a timely manner. When activating the emergency response system, please be mindful of the time the stroke symptoms began as it will aid in steadfast interventions for the patient. - Critical EMS assessments and actions:
Support ABC’s and give oxygen to patients if needed. Perform a prehospital stroke assessment. Assess the time of stroke onset and examine the patient at a stroke center, alerting the hospital in advance. This can activate the stroke team. Direct the patient to a CT Scan and check glucose levels, treating glucose if indicated. - Immediate assessment and stabilization:
Once the patient arrives at the emergency department, and within 10 minutes of arrival, inspect the vitals and provide oxygen if the patient is hypoxemic. Obtain run labs, IV access, and check glucose while performing neurologic screening with an emergent CT scan or MRI of the brain. Obtain a 12-lead ECG. - Assess neurologic assessment by stroke team or designee:
The stroke team or designee must review the patient’s history and create a timeline of symptom onset. Perform an examination using the NIH Stroke Scale. - Ensure the CT scan is completed within 20 minutes of arrival to the hospital or stroke center.
If detected with an ischemic stroke, then consider fibrinolytic therapy. If the CT scan shows no sign of hemorrhage, it is probable that the patient experienced an ischemic stroke and needs fibrinolytic therapy. This is when it is crucial to check for fibrinolytic exclusions such as head trauma, a history of intracranial hemorrhage, or active internal bleeding. Repeat the neurologic exam. This will assist in determining if a patient’s symptoms are worsening, improving, or staying the same. - Consult a neurologist and/or a neurosurgeon:
If the scan shows hemorrhage, consult neurologists or neurosurgeons, and start the stroke or hemorrhage pathway. - Review the risks and benefits with the patient and family:
Review the risks and benefits of fibrinolytic therapy with patient and/or family, if possible. Review within 1 hour of arrival and 3 hours of symptom onset. Administer rtPA and do not give anticoagulants or antiplatelets for 24 hours. The goal is to administer fibrinolytics before 1 hour of acquiring CT scan results. - Begin the post-rtPA stroke pathway:
Start the post-rtPA stroke pathway within 3 hours of symptom onset. Admit the patient to the stroke unit or intensive care unit and monitor blood pressure and neurologic deterioration.
Highlights of the ACLS Suspected Stroke Algorithm
The Advanced Cardiovascular Life Support (ACLS) suspected stroke algorithm is a systematic approach to managing patients suspected of having a stroke. Here are the key components:
- Recognition and Activation:
The very first thing is identifying the symptoms of a stroke, utilizing the FAST method, and pressing the alert button to trigger an emergency response. The FAST acronym is an approach that allows healthcare providers and lay persons to easily identify if a patient is experiencing a stroke.- Step 1. Ask the patient to smile. Does one side droop?
- Step 2. Ask the patient to close their eyes and raise both arms. Does one arm drift down?
- Step 3. Ask the patient to repeat a simple phrase. Does the patient’s speech seem slurred, garbled, or strange?
- Step 4. If you notice any of these symptoms, it is time to call the emergency responders. Please also notate the time the symptoms begin; this aids medical personnel to deliver the correct interventions.
- Supportive Care:
Administer supportive care, including keeping an open airway, sufficient breathing, and adequate circulation. With oxygen saturation less than 94%, the treatment should contain giving oxygen. - Transportation:
Timely transportation to the appropriate hospital is crucial to ensure prehospital notification and swift action. - Emergency Department Evaluation:
On hospital admission, perform a rapid evaluation of the patient, complete a neurological assessment and blood glucose; the CT scan will help differentiate between an ischemic and hemorrhagic stroke. - Stroke Team Assessment and Stroke Type Identification:
The stroke team will examine the patient to establish his or her type of blockage as well as recommend an effective treatment strategy. - Ischemic Stroke Treatment:
In the event of an ischemic stroke, time is imperative as prolonged blockage to necessary vessels in the brain can reduce a patient’s prognosis and delay healing, leading to reduction of symptoms. Sometimes, the doctor might even prescribe endovascular interventions. - Hemorrhagic Stroke Treatment:
If there is a hemorrhage on the scan, consult neurological experts and transfer the patient to a neurological ICU, if possible. Management of blood pressure, prevention of seizures, and appropriate consultation for surgical intervention is key to recovery. - Post-Acute Care:
Secondary prevention measures, rehabilitation, and treatment of any complications are the focus once primary treatment has been performed.
Want to keep the highlights handy? Download the ACLS Tachycardia Algorithm now.
Download ACLS Suspected Stroke Algorithm PDF
Sources
- https://linkinghub.elsevier.com/retrieve/pii/S0300957218301928
- van Walraven, C.; Stiell, I. G.; Wells, G. A.; Hébert, P. C.; Vandemheen, K. (November 1998). Do advanced cardiac life support drugs increase resuscitation rates from in-hospital cardiac arrest? The OTAC Study Group". Annals of Emergency Medicine. 32 (5): 544–553. doi:10.1016/s0196-0644(98)70031-9. ISSN 0196-0644. PMID 9795316. https://pubmed.ncbi.nlm.nih.gov/9795316/
- Jung, Julianna; Rice, Julie; Bord, Sharon (December 2018). "Rethinking the role of epinephrine in cardiac arrest: the PARAMEDIC2 trial". Annals of Translational Medicine. 6 (Suppl 2): S129. doi:10.21037/atm.2018.12.31. PMC 6330609. PMID 30740450. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6330609
- https://anesthesia.ucsf.edu/sites/anesthesia.ucsf.edu/files/wysiwyg/AcuteStroke.pdf
- Perkins, Gavin D.; Gräsner, Jan-Thorsen; Semeraro, Federico; Olasveengen, Theresa; Soar, Jasmeet; Lott, Carsten; Voorde, Patrick Van de; Madar, John; Zideman, David; Mentzelopoulos, Spyridon; Bossaert, Leo (2021-04-01). "European Resuscitation Council Guidelines 2021: Executive summary". Resuscitation. 161: 1–60. doi:10.1016/j.resuscitation.2021.02.003. ISSN 0300-9572. PMID 33773824. S2CID 232407605. https://www.resuscitationjournal.com/article/S0300-9572(21)00055-1/abstract
All ACLS Algorithms
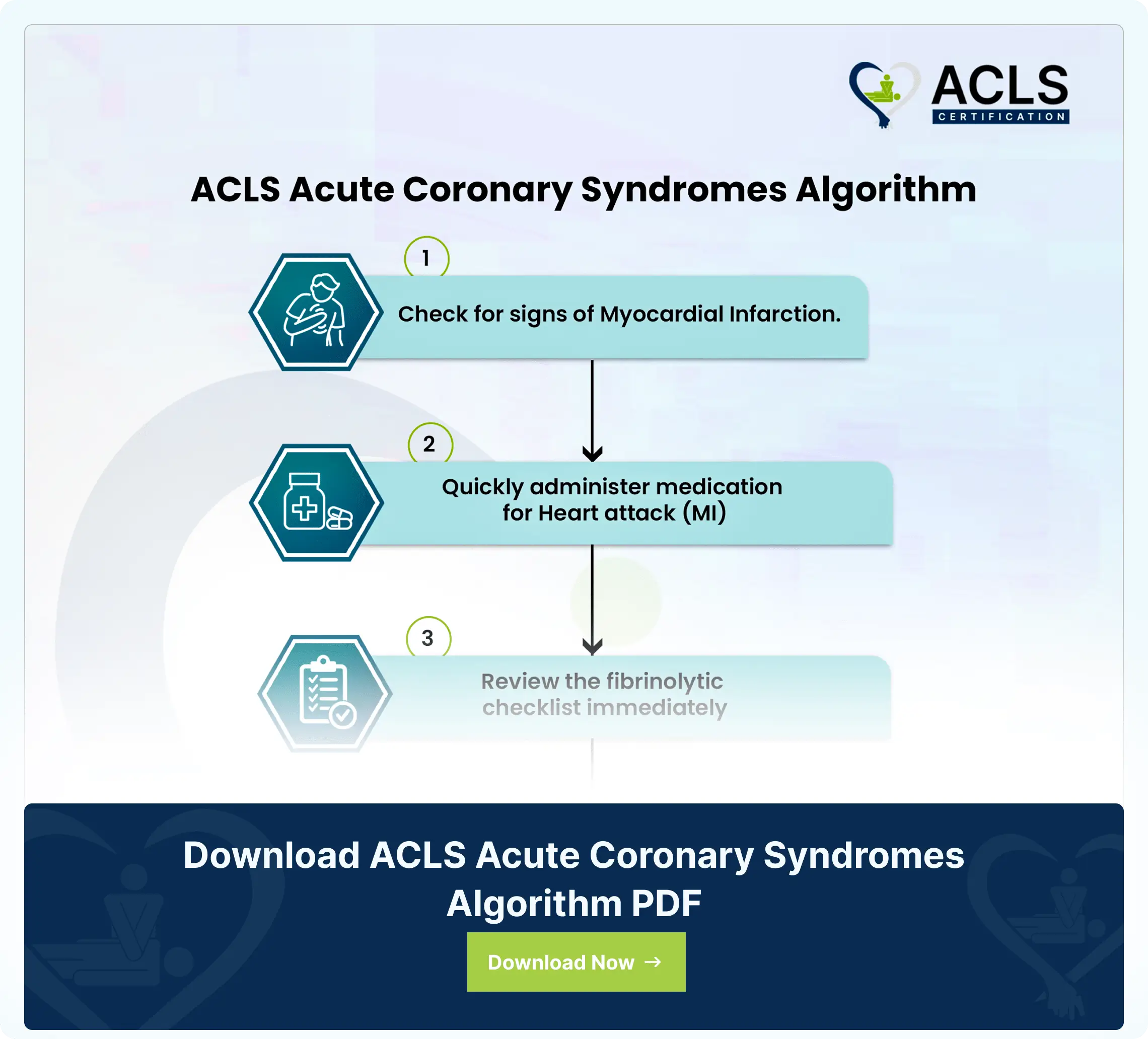
ACLS Acute Coronary Syndromes Algorithm
The ACLS Acute Coronary Syndromes Algorithm guides healthcare providers in the assessment, diagnosis, and treatment of patients with suspected or confirmed acute coronary syndromes
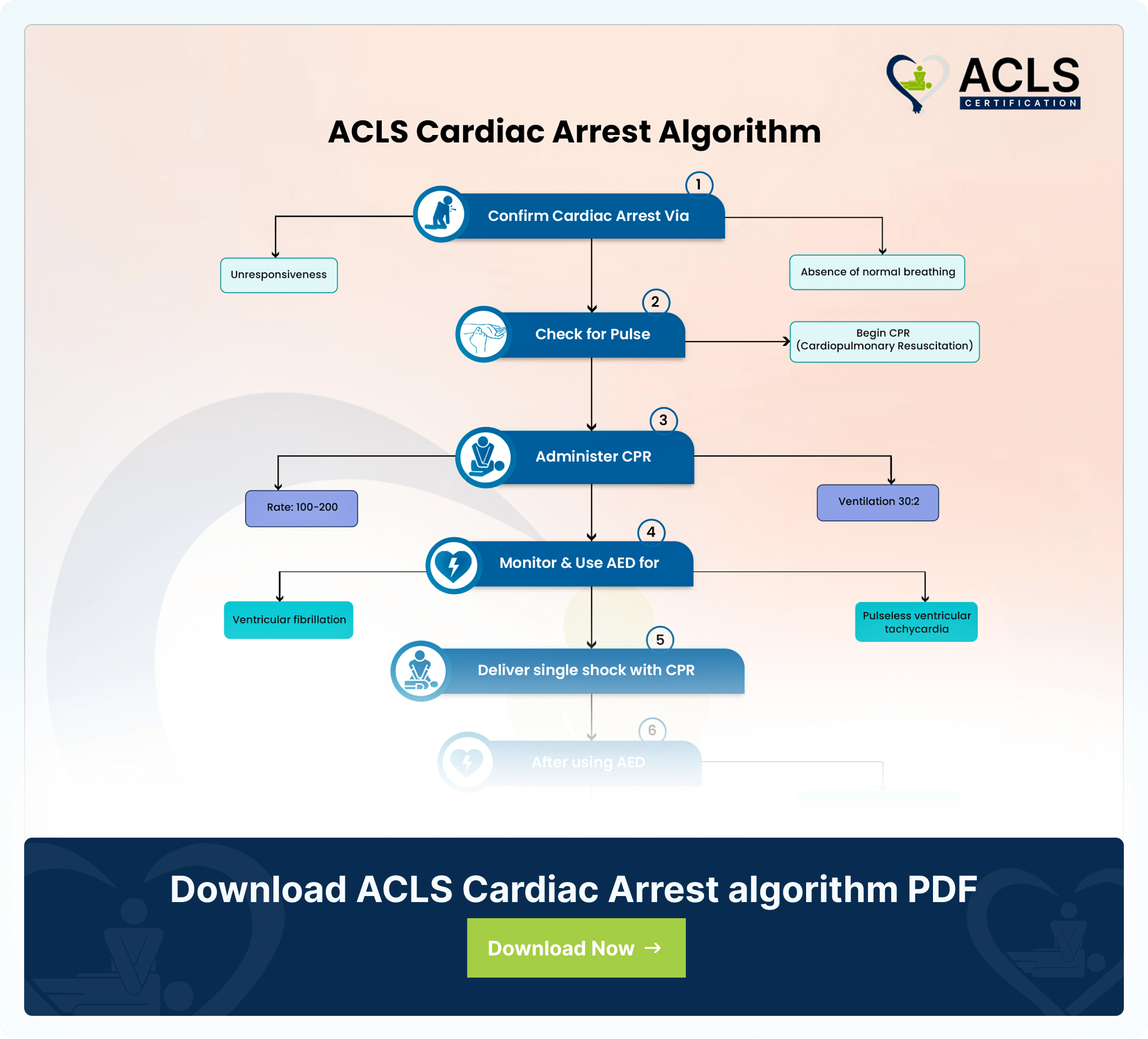
ACLS Cardiac Arrest Algorithm
The ACLS Cardiac Arrest Algorithm emphasizes CPR, defibrillation, drug therapy, and post-resuscitation care. It also highlights the importance of teamwork in optimizing outcomes during cardiac emergencies
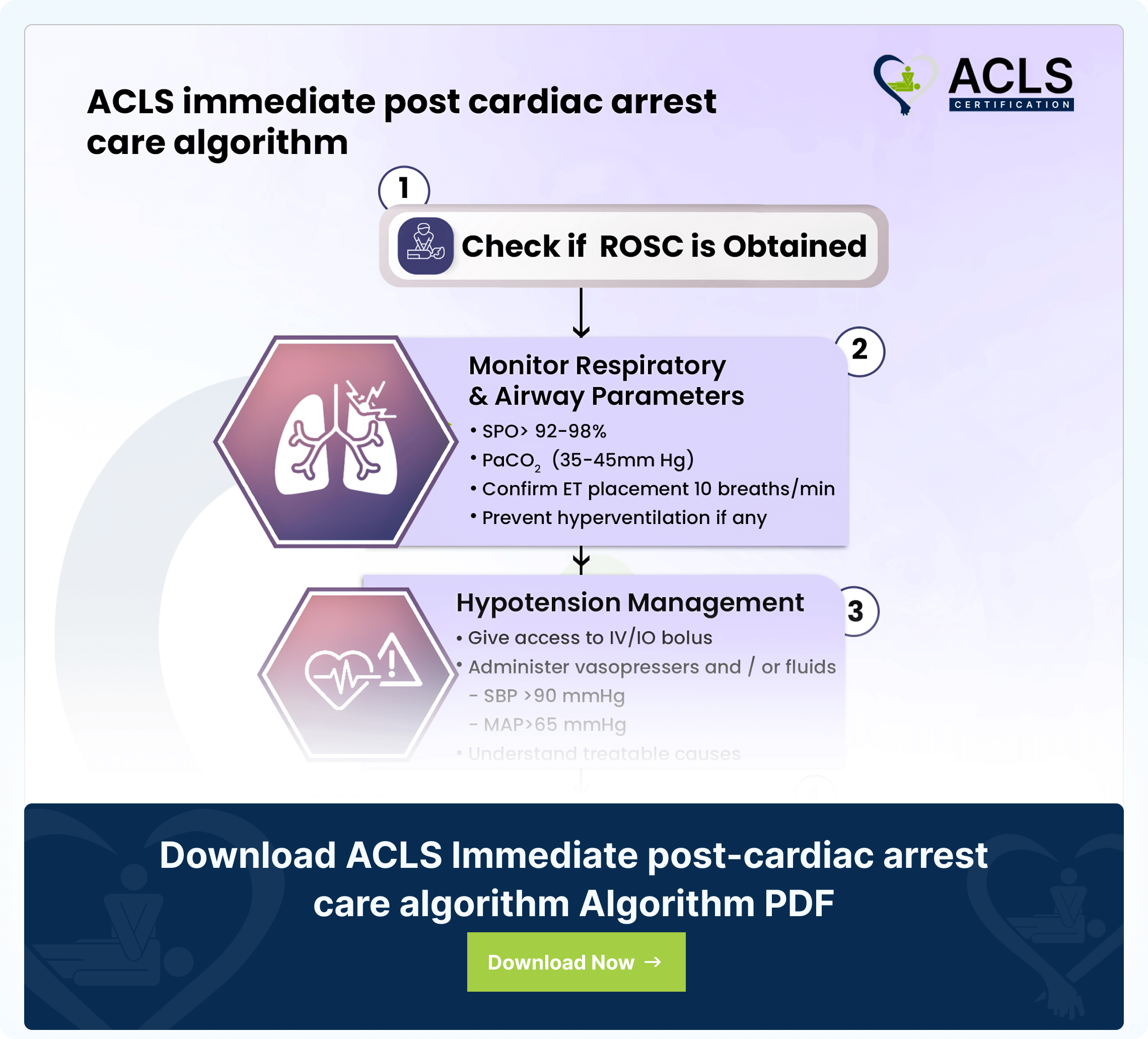
ACLS Immediate post-cardiac arrest care algorithm
The ACLS immediate post-cardiac arrest care algorithm guides critical interventions for patients post-resuscitation