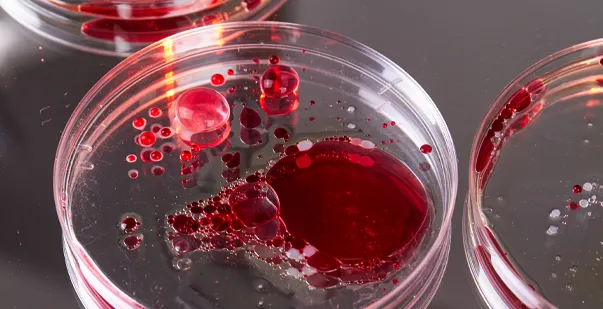
Bloodborne pathogens are microorganisms that can cause human illness and are present in human blood. Hepatitis B (HBV), hepatitis C (HCV), and the human immunodeficiency virus (HIV) are a few of these pathogens. Bloodborne pathogens can live for days or weeks in body fluids but cannot survive for long periods outside the body. Bloodborne pathogens may be exposed to workers through needlestick injuries and other sharps-related incidents. Thus, it is important to take steps to protect from bloodborne pathogens.
The biggest risk of infection is caused by contaminated needlestick sharps or possibly from using scalpels and sutures. Unprotected contact between a worker and other potentially infectious materials (OPIM) can also result in exposure. OPIM refers to blood contamination, unfixed tissues or organs, and bodily fluids. Preventing transmission thus starts with taking precautions for yourself.
Master ACLS Now
Get ACLS certified with confidence
How Can Bloodborne Pathogen Exposure Be Controlled?
An employer must implement an exposure control plan for the worksite that includes information on employee protection measures to lessen or eliminate the risks associated with occupational exposure to bloodborne pathogens. By OSHA’s Bloodborne Pathogens Standard, the plan must also outline how an employer will use engineering and work practice controls, PPE, employee training, medical surveillance, hepatitis B vaccinations, and other measures. The main strategy for preventing or reducing worker exposure is engineering controls, which include using safer medical equipment like plastic capillary tubes, shielded needle devices, and needleless devices.
Research indicates that up to one-third of all injuries caused by sharp objects happen during disposal. Since nurses are the ones who get needlestick injuries the most, they are especially vulnerable. According to estimates from the Centers for Disease Control and Prevention (CDC), using safer medical devices can prevent between 62-88% of injuries caused by sharp objects.
Read More: ACLS Acute Coronary Syndromes
Guidelines For Bloodborne Infections
OSHA bloodborne pathogens and personal protective equipment standards require employers to safeguard employees from exposure to infectious agents. Both employers and employees should understand several important infection control strategies, such as transmission-based, universal, and standard precautions.
-
Universal Precautions (UP):
They were introduced as an infection control strategy to shield workers from HIV, HBV, and other bloodborne pathogens in human blood and certain other body fluids, regardless of a patient’s infection status. Under the Universal Precautions for bloodborne pathogens, all human bodily fluids, including blood, are handled as though they were known to be infectious. However, the infection control community no longer employs UP alone, even though it is included in the BBP standard.
-
Standard Precautions (SP):
Added to the UP in 1996 as part of the “1996 Guideline for Isolation Precautions in Hospitals”, SP is a set of additional infection prevention measures designed to shield healthcare personnel from pathogens found in bodily fluids other than blood and other bodily fluids but also in human blood. Hand hygiene, the use of specific bloodborne pathogens PPE Kits depending on expected exposure, safe injection techniques, and the safe disposal of contaminated objects and equipment in the patient area are all included in SP. All patients receive SP treatment regardless of whether they are suspected or confirmed to be contagious.
-
Transmission-based Precautions (TBPs):
These actions serve to supplement standard preventive measures (SP) for contact, droplet, and airborne transmissible diseases with additional actions to obstruct the route(s) of transmission that SP alone might not be able to stop. Depending on what is known or suspected about a patient’s infection, different types of TBP are applied.
UP and body substance isolation principles were integrated into SP to cover what employers should do to shield employees from exposure. Other OSHA regulations, such as the Occupational Safety and Health Act’s PPE for bloodborne pathogens requirements, may also apply.
Several Key Elements of Risk-Reduction
The following are some crucial factors to take into account when lowering the risk of bloodborne infections:
-
Keeping Hands Clean
Maintaining clean hands is essential to stopping the spread of all contaminants, including BBPs. Healthcare organizations must ensure that employees flush their mucous membranes with water or wash their hands and any other skin with soap and water as soon as possible after coming into contact with blood or OPIM. Healthcare professionals should generally be aware of the locations of the nearest cleaning stations and how to properly and completely wash their hands.
-
Proper Placement of Sharps Containers
OSHA does not expressly specify the kind of container that an organization must use. However, potential exposures can be minimized or reduced using specially designed, puncture-resistant containers to safely store used needles, scalpels, broken glass, and other sharp items. Organizations should station sharps containers close to the patient care area to enable employees to properly and safely dispose of sharps afterwards.
-
Disposing of Personal Protective Equipment Properly
Personal Protective Equipment (PPE) is essential for preventing BBP exposure. Therefore, it must be easily accessible and available in suitable sizes for all healthcare workers. To prevent bloodborne pathogens PPE is an ideal tool, and it must be removed and put in a specified area or container to store, clean, decontaminate, or dispose of.
-
Extensive Instruction on Bloodborne Infections
Every employee who may be exposed to contaminants must undergo a thorough orientation and, at the very least, yearly refresher training covering the BBP Standard’s requirements. Employees should also receive additional training to reflect the increased occupational risks whenever new or modified tasks or procedures impact their occupational exposure.
Read More: ACLS Tachycardia Algorithms
Guarding Against Bloodborne Infection Exposure
The following are crucial actions that employers can take to shield their workers from bloodborne pathogen exposure:
- Safety Devices (Engineering Controls): Provide the best needlestick injury prevention devices, such as self-sheathing needles, sharps disposal containers, and needleless IV systems.
- Safe Work Practices: Teach and mandate that staff members adhere to safety procedures, such as wearing personal protective equipment (PPE), locking sharps disposal containers while in transit, and not recapping needles. Training workers on how to prevent bloodborne pathogens can also help a lot.
- Personal Protective Equipment (PPE): Wearing protective eyewear, face shields, gloves, and gowns of the highest caliber can all help shield employees from bloodborne pathogen exposure. To promote use, this equipment should be easily accessible.
- Hepatitis B (HBV) Vaccine for At-risk Workers: Although there is currently no vaccine against HIV or hepatitis C, all employees who may be exposed to bloodborne pathogens should have access to the highly effective hepatitis B vaccine. OSHA mandates that employers should provide their workers with access to this vaccine.
Exposure to bloodborne pathogens can also result in psychological harm. Employers who keep the lines of communication open, educate their staff about exposure, and assist them while they receive treatment can all help reduce employee fear and anxiety.
The Right PPE For Preventing Bloodborne Infections
To protect yourself against all bloodborne diseases, you must have appropriate personal protective equipment and apparel. This implies that the protection must be suitable for the anticipated exposure. For instance, a lab technician taking blood only needs gloves, but a pathologist doing an autopsy would require far more protective gear.
- PPE can include lab coats, pocket masks, face shields or masks, gloves, gowns, and other protective clothing. Employees must have easy access to the equipment and be able to get the right size.
- Employees must wear gloves if they are expected to come into contact with blood, other potentially infectious materials, or contaminated surfaces with their hands. Gloves intended for one use cannot be cleaned or recontaminated.
- If utility gloves are not compromised, they could be decontaminated. When they exhibit signs of deterioration, such as peeling, tearing, puncturing, or cracking, they ought to be replaced.
- If workers have allergies to regular gloves, the employer must supply hypoallergenic gloves or comparable substitutes. While wearing proper gloves is required for all other professionals who collect blood samples (phlebotomies), it is not necessary at voluntary blood donation centers.
- Gloves are required for employees working in voluntary blood donation centers in three situations: (1) when they have cuts, scratches, or other skin breaks, (2) during training, and (3) when they suspect contamination.
- When potentially infectious materials spray, splatter, or droplet particles pose a risk to the eyes, nose, or mouth, workers should wear protective goggles, masks, glasses with solid side shields, and masks or chin-length face shields.
- When severe contamination is anticipated, more comprehensive protection, such as gowns, aprons, surgical caps and hoods, shoe covers, or boots. For instance, this frequently happens during orthopedic surgery or autopsies.
Employers are required to supply the PPE and ensure that employees wear it. In addition to cleaning or laundering apparel and equipment, the employer must fix or replace it as needed.
Facilities conducting HIV or HBV research must implement additional bloodborne precautions for safety, such as using personal protective equipment (PPE) in animal rooms and disinfecting PPE before laundering.
Exception To Requirement For PPE
There is one situation in which wearing protective gear is optional.
- An employee may forgo the equipment, albeit momentarily and under exceptional circumstances.
- The employee’s professional judgment must determine whether donning the protective gear would increase the risk to their own or their coworkers’ safety or prevent the provision of medical care or public safety services.
- Employers must look into and record the circumstances when one of these exempt situations happens to see if there is a way to prevent it.
Precautions to Take if You Are Exposed to Infection
Here is how to protect yourself from bloodborne pathogens if you encounter a bloodborne infection. Take the following safety precautions:
- Clean any cuts, wounds, or exposed skin after using soap and water to prevent needlestick injuries.
- Rinse the area around the mouth and nose with water if blood or anything potentially infectious is splashed there.
- If splashed in or near the eyes, rinse for 20 minutes using sterile irrigants, saline water, or clean water.
- Please inform the relevant person mentioned in your employer’s exposure control plan about the incident immediately. Also, please inform the emergency medical services (EMS) staff who also take over for you about the incident.
- Note down what transpired to document the incident. Add any actions you took following the exposure, the date, time, and circumstances of the exposure, as well as any other information your employer requires.
- Seek out the prompt follow-up care that your employer has specified in their exposure control plan.
Final Thought
Serious concerns about bloodborne infections arise in healthcare environments. By adhering to standard precautions and developing an exposure control plan, you can safeguard against the unintentional spread of bloodborne pathogens and other infectious materials in healthcare. The Standard Precautions principle, also known as Universal Precautions, is one of the best ways to protect from bloodborne pathogens.
All human bodily fluids, including blood, are assumed to be infectious and should be handled with the proper precautions. This is the basis of standard precautions. It is imperative to take all reasonable precautions to prevent bloodborne infections because certain pathogens have no known treatment, and others cannot be prevented through vaccination. Above all, if you have the chance to come into contact with blood or bodily fluids, always wear personal protective equipment (PPE) like gloves and eye protection.