Table of content(s)
- Introduction
- What are the key differences in the origin of SVT and VT within the heart?
- How do the symptoms of SVT and VT differ in terms of severity?
- What are the distinct electrocardiogram (ECG) findings that help differentiate SVT from VT?
- How does the left ventricular ejection fraction (LVEF) vary between SVT and VT cases?
- What are the implications of SVT and VT on the structural and functional changes in the heart?
- How effective are the current diagnostic algorithms in discriminating between SVT and VT in chronic cases?
- What treatment strategies are recommended for managing SVT and VT?
- Conclusion
Supraventricular Tachycardia (SVT) and Ventricular Tachycardia (VT) differ in origin and severity. SVT originates above the heart’s lower chambers, while VT starts in the ventricles, the heart’s primary pumping chambers.
VT can have more severe and life-threatening symptoms due to its location. Studies show that VT can lead to a huge decrease in left ventricular ejection fraction compared to SVT. Learning the distinction between SVT and VT is crucial for appropriately treating these heart rhythm disorders. The latest ACLS guidelines recommend stabilizing the patient and treating reversible causes of wide QRS complex tachycardia. So, let us explore more SVT vs VT and the recommended strategies for managing them.
What are the key differences in the origin of SVT and VT within the heart?
Here are the key differences based on origin between Supraventricular Tachycardia (SVT) and Ventricular Tachycardia (VT).
| Feature | Supraventricular Tachycardia (SVT) | Ventricular Tachycardia (VT) |
| Origin of Tachycardia | Upper chambers (atria) | Lower chambers (ventricles) |
| Severity | Less severe | More severe and life-threatening |
| Diagnosis | >80% of narrow complex tachycardia | >80% of wide QRS tachycardias |
| S1 Intensity (ECG) | Higher | Lower |
| S1 Variability (ECG) | Lower | Higher |
| Common in | Newborns, infants, congenital heart disease | Any age |
| Incidence in Adults with Congenital Heart Disease | Up to 50% (increases with age/surgery time) | Less common than SVT |
How do the symptoms of SVT and VT differ in terms of severity?
Symptoms of Supraventricular Tachycardia (SVT) and Ventricular Tachycardia (VT) differ in severity. SVT comes with palpitations, while VT shows more severe symptoms. Let us take a look at the difference:
SVT:
- Palpitations are common (22% of cases)
- Chest pain (5%), syncope (4%), and sudden cardiac death (0.4%) are less frequent
VT:
- Palpitations are reported in only 8.8% of VT patients
- Patients with VT often experience chest pain (64%), dyspnea (21%), and dizziness (26%)
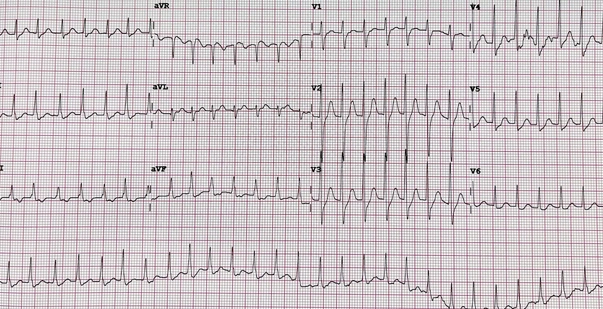
What are the distinct electrocardiogram (ECG) findings that help differentiate SVT from VT?
Several findings can help tell the difference between SVT and VT on ECG. SVT is shown by S1 intensity along with a certain degree of variability. On the other hand, VT is indicated by AV disintegration and RWPT >50 ms in the second lead.
Algorithms like Vereckei and Brugada can also help distinguish between SVT and VT. Vagal maneuvers can differentiate SVT (responds) from VT (does not respond). The surface ECG is crucial for diagnosing arrhythmias, with a systematic approach increasing accuracy to over 95%. VT and SVT differences are also seen in certain ECG findings.
Read more: A Guide to Understanding ECG Artifacts
How does the left ventricular ejection fraction (LVEF) vary between SVT and VT cases?
Left ventricular ejection fraction (LVEF) varies between SVT and VT cases as follows:
- SVT cases show a significantly higher LVEF compared to VT cases.
- In SVT, the LVEF was found to be around 67.1%, while in VT cases, it was lower at 23%.
- The difference in LVEF between SVT and VT cases can help differentiate between the two arrhythmias.
What are the implications of SVT and VT on the structural and functional changes in the heart?
Here are the implications of SVT and VT on the structural and functional changes in the heart.
- SVT if acute results in dysfunction of LV. It shows a decrease in LV fractional shortening.
- In contrast, VT can cause hemodynamic instability, heart failure, and even sudden cardiac death, especially in the presence of structural heart disease
- SVT results in LV hypertrophy and increased collagen content, while VT may lead to tachycardia-induced cardiomyopathy and hemodynamic collapse
- SVT and VT have distinct effects on the heart’s structure and function. This makes timely management important.
How effective are the current diagnostic algorithms in discriminating between SVT and VT, especially in chronic cases?
Current diagnostic algorithms show varying effectiveness in discriminating between SVT and VT. The Brugada and Vereckei algorithms have been widely used but may have limitations in certain populations.
Newer methods like the RS/QRS ratio and the Basel algorithm have shown high accuracy in discriminating SVT from VT, with sensitivities up to 97.2% and specificities up to 90%. These algorithms offer improved diagnostic performance, especially in challenging cases, providing rapid and accurate differentiation between SVT and VT.
What treatment strategies are recommended for managing SVT and VT?
Here are the recommended treatment strategies:
For SVT:
- Vagal maneuvers like the Valsalva maneuver and carotid sinus massage are recommended.
- Adenosine or epinephrine can be used if vagal maneuvers don’t work.
- Compression treatment and fondaparinux may be needed in certain cases
For VT:
- Catheter ablation is a primary treatment for VT.
- A few antiarrhythmic medications and implantable cardioverters also prove beneficial.
Read more: Study Guide To Body Systems: ACLS Certification Resource
Conclusion
SVT vs VT differ in origin, symptoms, and severity. VT originates in the ventricles, leading to more severe symptoms like chest pain and dyspnea. ECG findings, LVEF, and structural changes help differentiate SVT (higher LVEF) from VT. Diagnostic algorithms like Vereckei and Brugada aid in accurate discrimination. Treatment includes vagal maneuvers for SVT and catheter ablation for VT. Thus, understanding these differences is crucial for the effective management of these heart rhythm disorders.