Have you ever felt your heart beating slower than usual? These could be signs of a condition called Second-Degree AV Block Type I or second-degree heart block type 1. Think of your heart as an electrical powerhouse, with signals traveling from the atria to the ventricles to keep it pumping rhythmically. In the second-degree atrioventricular block, some of those signals get delayed or blocked along the way. Recognizing the symptoms of this “Wenckebach” or “Mobitz I” block is crucial. Let’s dive in and learn how to spot the signs before they potentially lead to more serious issues.
What is Second-Degree AV Block Type I?
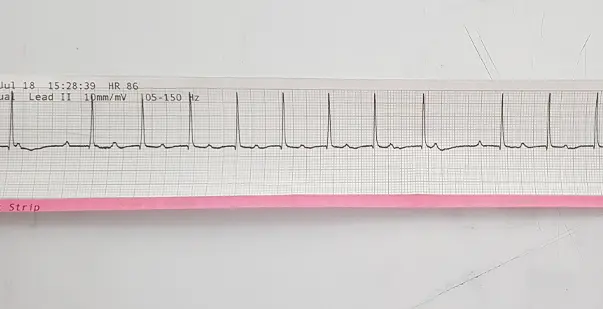
Second-degree AV block type I sporadically blocks electrical impulses from the upper to lower heart. ECGs reveal this block as a prolonged PR interval and skipped beats. Aging, cardiac disease, and certain drugs may impede AV node signal transmission. It is considered moderate and less likely to cause a complete heart block than other forms.
Signs and Symptoms of Second-Degree AV Block Type I
Second-degree AV Block Type I might not always cause symptoms. However, it’s important to recognize the signs. These can range from mild changes in heart rate and blood pressure to symptoms like dizziness, fainting, and chest pain. Knowing these signs and symptoms may help in early recognition and treatment.
Bradycardia
Sinus bradycardia with second degree is when the heart beats slower than normal. It is a common sign of Second-Degree AV Block Type I. This occurs because the heart block 2nd degree type 1 intermittently delays the electrical signals as they reach the ventricles. This delay, characteristic of 2nd Degree AV Block Type, results in a slower heart rate.
Hypotension
Blood pressure below normal is hypotension. It can sometimes occur with second-degree AV block type 1 or 2nd degree type 1. This happens because the heart cannot pump blood efficiently, and the decreased rhythm in the ventricles contributes to this issue.
Dizziness or Light-headedness
Patients with 2nd degree heart block type 1 may experience dizziness or lightheadedness. These symptoms are often caused by a temporary drop in blood pressure due to the delayed movement of electrical signals.
Syncope
Syncope is when someone faints due to a sudden drop in blood pressure. It can happen in severe cases of the mobitz 2. This condition occurs when the heart does not pump enough blood to the brain.
Chest Pain
While it is rare, some people with Type I Second-Degree AV Block might feel chest pain or discomfort. This can happen because the heart is working harder to compensate for the delays in electrical signal conduction.
It’s also important to note that some people with Second-Degree AV Block Type I may not show any symptoms. They might not realize they have the condition, and it could be found by accident during an electrocardiogram (ECG) or a regular check-up.
Diagnosis of Second-Degree AV Block Type I
Doctors use an electrocardiogram (ECG) to diagnose second-degree AV block type I. This noninvasive test records the heart’s electrical activity and helps show how signals move between the atria and ventricles.
The ECG analysis of Second-Degree AV Block Type I will unveil a distinctive pattern referred to as the Wenckebach block phenomenon. The PR interval shows the time delay between the electrical impulse from the atria and the contraction of the ventricles. In this pattern, the PR interval slowly gets longer. As it extends, the QRS complex, which indicates ventricular contraction, may be reduced or even missed.
The PR interval gets longer over time, and then a QRS complex disappears. This pattern on an ECG confirms Type I Second-Degree AV Block. In some cases, doctors may do more tests. These help check the condition further and rule out other possible causes. Potential testing that may be conducted comprises:
- Exercise stress testing: To evaluate the impact of heightened physical activity and stress on cardiac performance.
- Holter monitoring: A portable device designed to record the electrical activity of the heart continuously for a prolonged duration, typically ranging from 24 to 48 hours.
- Echocardiogram: An ultrasound examination that provides comprehensive data regarding the structure and function of the heart.
While these additional tests may give useful information, the ECG is still the primary diagnostic tool for diagnosing and differentiating Second-Degree AV Block Type I from other forms of heart blockages.
Treatment of Second-Degree AV Block Type I
The treatment for Type I Second-Degree AV Block depends on its severity and cause. People with no symptoms or just a slow heart rate may not need treatment. This is especially true if their condition is mild.
If the patient shows clear symptoms or if the block is severe, treatment may be needed. This controls the disease and prevents problems. Possible treatments include the following:
- Medication Adjustments: If medications like calcium channel blockers or beta-blockers are causing the block, doctors may change them. This is done under medical care to help lessen the block.
- Treatment of Underlying Conditions: Sometimes, a heart block comes from other health issues. These could be thyroid disorders, electrolyte imbalances, or heart diseases. Treating these conditions can help fix the block.
- Pacemaker Implantation: In severe cases of Second-Degree AV Block Type I, doctors may recommend a permanent pacemaker. This is especially true if the condition causes symptoms or is worsening. The device is placed under the skin. It helps control the heart’s electrical signals, ensuring the heart beats regularly and normally.
Conclusion
Early diagnosis and treatment of Second-Degree AV Block Type I require recognizing its symptoms. Some instances are asymptomatic, while others cause dizziness, fainting, or chest discomfort. If you or someone you know has signs of a second-degree AV block, see a doctor immediately. Early identification and treatment may avoid problems and improve heart health.