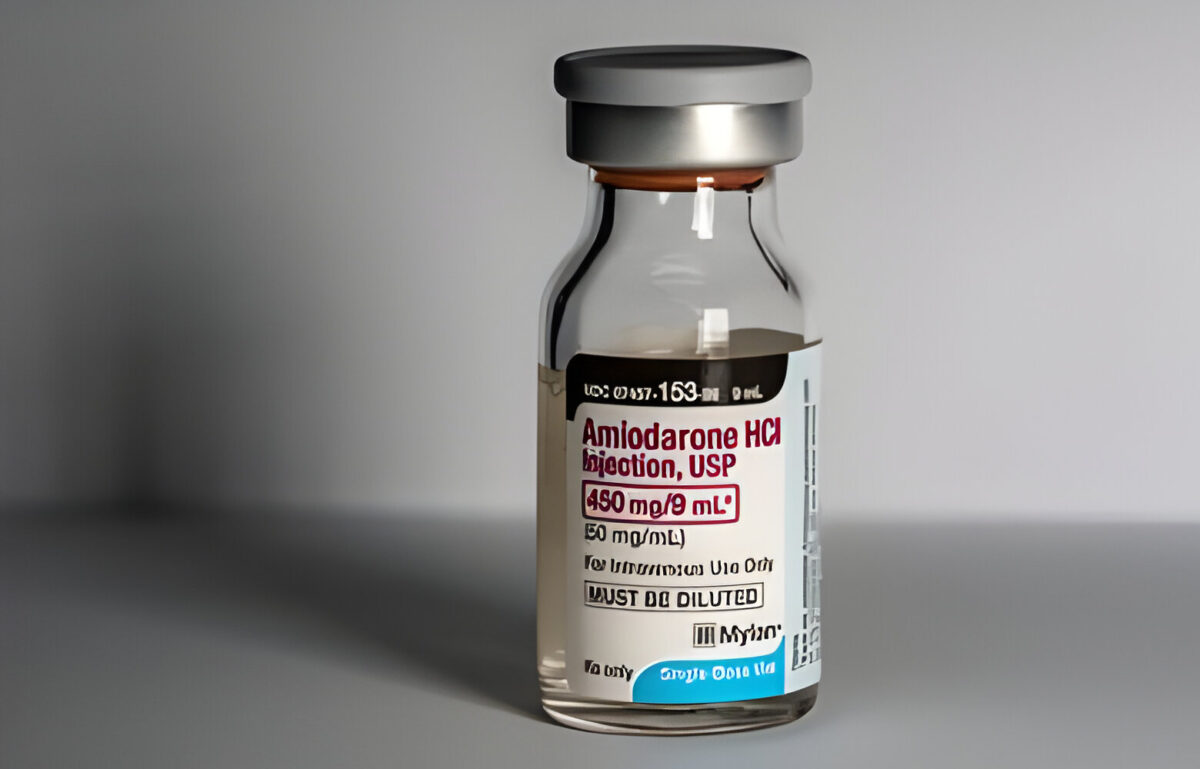
Amiodarone is an antiarrhythmic medication. It helps restore normal heart rhythms during cardiac emergencies. It has a unique mechanism of action, which regulates heart rhythm disturbances. In ACLS, Amiodarone is administered intravenously, with a dosage adjustment that is based on the patient’s condition.
While it is highly beneficial, it’s also important to be aware of the potential side effects of Amiodarone. These include lung and thyroid problems. Nevertheless, amiodarone and ACLS is a vital tool that offers a lifeline in critical situations like cardiac arrest, and arrhythmias. So, let us explore and understand more about the medication.
Master ACLS Now
Get ACLS certified with confidence
What is Amiodarone and How Does it Work?
Amiodarone is an antiarrhythmic medication used to treat irregular heartbeats.
Here is how it Works:
- Amiodarone stabilizes the heart’s electrical activity.
- It blocks certain electrical signals in the heart to restore normal rhythm.
- Amiodarone also relaxes blood vessels, improving blood flow.
- By regulating heart rhythm, it helps prevent life-threatening arrhythmias.
Read More: ACLS Certification in Ohio
What are the Recommended Doses for Amiodarone?
Let’s learn about the recommended doses of Amiodarone in treating cardiac arrhythmias.
| Patient Population | Loading Dose (mg) | Maintenance Dose (mg/day) |
| Adults | 8001600 | 400 |
| Pediatrics | 5 mg/kg | 5 mg/kg |
| Elderly | 400600 | 200300 |
| Renal Impairment | 400800 | 100200 |
| Hepatic Impairment | 600800 | 100200 |
These doses vary based on individual patient factors and are adjusted accordingly.
Read More: Acls promo code
What is the Mechanism of Action of Amiodarone?
Understand how Amiodarone exerts its therapeutic effects through its unique mechanism of action.
Ion Channel Blockade:
- Amiodarone blocks potassium, sodium, and calcium ion channels in cardiac cells.
- This action prolongs action potential duration and refractory periods, preventing arrhythmias.
Beta Adrenergic Blockade:
- Amiodarone antagonizes beta-adrenergic receptors, reducing sympathetic activity.
- This decreases heart rate and contractility, stabilizing cardiac rhythm.
Alpha Adrenergic Blockade:
- Amiodarone also inhibits alpha-adrenergic receptors, leading to vasodilation.
- This reduces systemic vascular resistance, improving blood flow and decreasing cardiac workload.
Anti Arrhythmic Effects:
- Overall, Amiodarone’s multi channel blockade and antiadrenergic properties help to restore normal cardiac rhythm.
- This makes it effective in treating various arrhythmias.
Read more: Resuscitation Triangle Team Roles in ACLS
What are the Key Benefits of Using Amiodarone in ACLS?
Discover the key benefits of incorporating Amiodarone into ACLS protocols.
- Restores normal heart rhythm during life-threatening arrhythmias.
- Provides rapid and sustained suppression of ventricular arrhythmias.
- Reduces the risk of ventricular fibrillation or ventricular tachycardia.
- Enhances cardiac output by optimizing heart rhythm and function.
- Improves overall survival rates in patients experiencing cardiac arrest.
- Optimal treatment for various arrhythmic emergencies in diverse patients.
How Does Amiodarone Compare to Other ACLS Medications?
Here are the key differences between Amiodarone and other ACLS medications.
| Medication | Amiodarone | Lidocaine | Epinephrine |
| Mechanism | Multichannel blockade, antiadrenergic effects | Sodium channel blocker, antiarrhythmic | Alpha and beta adrenergic effects |
| Indications | Ventricular arrhythmias, supraventricular tachycardia | Ventricular arrhythmias | Cardiac arrest, anaphylaxis |
| Dosage | Loading: 8001600 mg, Maintenance: 400 mg daily | Loading: 11.5 mg/kg, Maintenance: 14 mg/min, titrated to effect | IV: 1 mg every 35 minutes during resuscitation |
What are the Potential Side Effects of Amiodarone?
The potential side effects of amiodarone include:
- Pulmonary toxicity, including interstitial pneumonitis and pulmonary fibrosis.
- Thyroid dysfunction, such as hypothyroidism or hyperthyroidism.
- Hepatotoxicity presents as elevated liver enzymes or hepatitis.
- Ocular complications, including corneal deposits or optic neuropathy.
- Skin reactions, such as photosensitivity or blue-gray discoloration.
- Neurological effects, including peripheral neuropathy or ataxia.
- Cardiovascular effects, such as bradycardia or QT prolongation.
- Gastrointestinal disturbances, including nausea, vomiting, or constipation.
How Does Amiodarone Improve ACLS Outcomes
Discover how Amiodarone contributes to improved outcomes in Advanced Cardiac Life Support (ACLS) scenarios.
- Restores and stabilizes normal cardiac rhythm during life-threatening arrhythmias.
- Suppresses ventricular arrhythmias rapidly and effectively.
- Reduces the risk of recurrent ventricular fibrillation or ventricular tachycardia.
- Enhances cardiac output and perfusion by optimizing heart rhythm and function.
- Increases the likelihood of successful resuscitation and survival rates in cardiac arrest situations.
- Provides a reliable treatment option for various arrhythmic emergencies, improving overall patient outcomes.
Read more: Elements of Effective Team Dynamics in ACLS
Conclusion:
Amiodarone plays a major role in ACLS. Amiodarone and ACLS together offer important interventions for cardiac emergencies. Despite its side effects, understanding its mechanisms and benefits is essential for optimal patient care. By leveraging Amiodarone’s efficacy in restoring normal heart rhythms and enhancing survival rates, healthcare providers can navigate ACLS scenarios with confidence.